Article / Case Study
1Regional Emergency Medical Services, RAV Brabant Midden-West-Noord, ‘s-Hertogenbosch, the Netherlands.
2Department of Cardiology, Maastricht University Medical Center, Maastricht, the Netherlands.
3Department of Anesthesiology, Erasmus University Medical Center—Sophia Children’s Hospital, Rotterdam, the Netherlands.
4Department of Cardiology, Zuyderland Medical Centre, Heerlen, the Netherlands.
5Cardiovascular Research Institute Maastricht (CARIM), the Netherlands.
6Department of Cardiology, Jeroen Bosch Medical Center, ’s-Hertogenbosch, the Netherlands
Risco C. W. van Vliet,
Regional Emergency Medical Services, RAV Brabant Midden-West-Noord,
Gruttostraat 14, 5212VM, s-Hertogenbosch,
The Netherlands.
Slovakia.
20 April 2025 ; 26 May 2025
Electrical cardioversion is the preferred treatment for unstable patients with life-threatening tachyarrhythmia. However, this can only be done if the patient is unconscious or sedated. In the case of a conscious patient experiencing cardiogenic shock due to broad-complex tachycardia in a prehospital setting, the pharmacologic treatment options are limited according to the Dutch national ambulance protocol. This is because Dutch ambulance nurses are not authorized to administer sedation without assistance from a physician-staffed service such as Helicopter Emergency Medical Services (HEMS). Unfortunately, physician-staffed services may not always be available. Therefore, there is a need for trained ambulance personnel who are capable of performing these procedures. Fortunately, nurse practitioners and physician assistants have emerged as viable care provider within Dutch ambulance care for several years now. These advanced practice providers (APP) are medically trained professionals and authorized to perform certain treatments and procedures that are supplementary to the ambulance process, including providing sedation. Yet not many ambulance services in the Netherlands are already using APP in patient care and implementation strategies are still being diligently sought. This case study highlights the life-saving potential of an APP within an ambulance service in the south of the Netherlands.
Case summary A 75-year-old man collapses while celebrating Carnival. His skin tone is pale and he is sweating profusely. His friends call the National emergency number and an APP arrives first at the scene. The man lies on the street in an overcrowded city center in front of a pub. The man has broad-complex tachycardia and is in cardiogenic shock with reduced responsiveness but still conscious. These life-threatening signs require immediate intervention and together with the ambulance team the APP creates a treatment plan. Instead of the treatment described in the national ambulance protocol, the APP decides on immediate cardioversion. After administering the sedation, synchronized cardioversion is performed once with 150 joules. After this, the parameters stabilize and the man is taken to a cardiac care unit in the nearest hospital with sinus rhythm and no adverse signs.
Discussion The case shows that direct cardioversion under sedation is feasible instead of drug treatment with a class III antiarrhythmic agent (amiodarone) and urgent transport with a patient who is in cardiogenic shock, with a high chance that a resuscitation situation would arise. This demonstrates the life-saving action of an APP. This perspective can provide new insights into prehospital treatment strategies for patients with arrhythmias.
Keywords: Ambulance, Emergency medical service, Advanced practice providers, Broadly complex tachycardia, Case report
In cases of cardiogenic shock due to an abnormal heart rhythm, rapid intervention is life-saving. international guidelines also prescribe rapid cardioversion for broadly complex tachycardia. However, this has prehospital limitation because the professionals working there do not have these skills. Where possibly a nurse practitioner could and should.
This case study postulates the important role a nurse practitioner can take and therefore be life-saving for a small group of patients in need. This article can be inspirational for other ambulance services in the Netherlands as in the world.
The Dutch Emergency Medical Services (EMS) are highly organized, with ambulance crews consisting of a specialized nurse and an ambulance driver. These ambulance nurses undergo an 18-month dedicated training program and are licensed to independently administer advanced life support level medical treatment. In their practice, they are supported by a national ambulance protocol (Ambulancezorg Nederland, 2024; Backus et al., 2020) The national protocol is a tool to achieve good ambulance care with an emphasis on offering support to the ambulance care professional in making decisions about appropriate care for an individual patient in a specific situation. However, this decision must fit the authority and expertise of this ambulance professional. Starting in 2020, the “Pilot Physician’s Assistant and Nurse Practitioner Ambulance Care” framework has provided guidance for the implementation of Nurse Practitioners (NPs) and Physician Assistants (PAs) in Dutch ambulance care (Ambulancezorg Nederland, 2020). The number of these advanced practice providers (APP) has been steadily increasing, granting them a significant role in prehospital care. Acknowledging their skills and legal capabilities, the APPs perform medical procedures outlined in both national protocols and international guidelines while ambulance nurses must adhere to national protocol. van Vliet et al. (2022). The presented case highlights a scenario in which care based on the national standard ambulance protocol is suboptimal, and demonstrates how adherence to international Advanced Life Support (ALS) guidelines by an APP can be life-saving. The primary objective of this report is to raise awareness of the treatment options provided by an APP by aligning with international ALS guidelines when the national protocol proves insufficient.
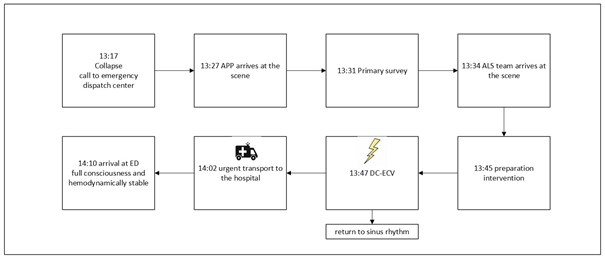
The information below is taken from the dispatch center report form and ambulance run sheet and is presented in chronological order. 13:17 Call from the ambulance dispatch center to the Solo rapid responder unit, staffed with an APP. Figure 1 a rendering of this notification.
| 75 years old, male, awake, self-breathing. Chest Pain (Non-Traumatic), difficulty speaking between breaths. Statement reporter: musician 75 years old, patient with previous cardiac history, suffering from chest pain and got not well suddenly. His skin is pale. He is fully awake. He has difficulty breathing normally. He has difficulty talking between breaths |
|---|
Figure 1: Notification from the emergency dispatch center
75 years old, male, awake, self-breathing. Chest Pain (Non-Traumatic), difficulty speaking between breaths. Statement reporter: musician 75 years old, patient with previous cardiac history, suffering from chest pain and got not well suddenly. His skin is pale. He is fully awake. He has difficulty breathing normally. He has difficulty talking between breaths 13:27 Within ten minutes the APP had arrived. The man had played the trumpet in a band during a Dutch carnival festival. During two days he had experienced pain in his left shoulder but did not pay any attention to it. Celebrating carnival, he suddenly felt severe backpain, felt very sick, and collapsed in front of his fellow musicians. He had a very tight feeling around the chest and had perspired heavily. His friends carried him to a quieter area, and despite the challenging conditions—open air, crowds, and noise—the APP systematically assessed his vital signs during the primary survey. See table 1 and Figure 2.
Table 1: Primary Survey
| tracts | findings | actions |
|---|---|---|
| Airway | Clear | |
| Breathing | Superficial, accelerated, SpO2 via finger clip is not measurable | The patient was immediately given a non-rebreathing mask with 15 liters of oxygen |
| Circulation | There is no palpable pulsation at the radial artery, scoop: broad complex tachycardia 220/min and clinical presentation of shock. | An 18 gauche infusion in the brachial vein is placed and infusion with 500cc of Ringers. |
| Central nervous system | Consciousness is decreased with EMV-score 11 (3 Eye- opening, 6 best Motor response, 2 best Verbal response) |
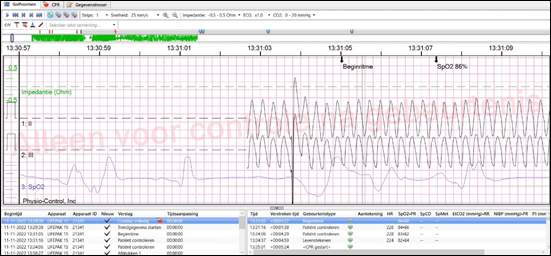
Figure 2: Initial rhythm
The APP recognized the seriousness of the situation and requested support from an EMS unit with advanced life support capacity. Due to the patient’s instability and profusely sweating, performing a 12-lead ECG was not feasible, so the APP focused on immediate action.
13:34 The ambulance team arrived and together with the APP they made a treatment plan. Dutch ambulance protocol dictates to administer 300 milligrams of Amiodarone intravenously, via a mechanical infusion pump in 15 minutes, in the situation of a wide-complex tachycardia in which the patient is responsive. Meanwhile, proceed with emergency transport to the nearest hospital with cardiac care (Ambulancezorg Nederland, 2016). Because of the hypotension, and/or the presence of presyncope, the APP was convinced that the man could go into a resuscitation situation at any moment and that amiodarone would not likely result in prompt cardioversion, so a different plan had to be made. The APP deviated from the Dutch national protocol and suggested a different treatment. The ability to administer sedation allowed the APP to treat the patient according to the latest international guidelines (Dresen et al., 2018; Domanovits et al., 1999). The APP assumed that the patient had recently consumed food and liquids, which posed a known risk during the procedure. Suction and airway devices were placed within reach and supported by consultations with the medical manager, and preliminary preparations began.
13:45 Defi-pads were placed in anterior and lateral positions and the lifepack© was set on synchronous defibrillation (= cardioversion). After an initial gift of 0.5mg/kg and titration until the man lost consciousness, the man was sufficiently sedated after a total of 80mg of propofol. He was no longer conscious but had respiration of his own. The APP ordered the ambulance nurse to perform a single synchronized cardioversion with biphasic 150 joules and after the shock, the rhythm immediately returned to a sinus rhythm of 89/min. The patient was in a supine position but still unconscious from the sedation. At that moment, the patient vomited heavily and was immediately turned onto his side to clear his airway. Within 5 minutes the man returned to a state of consciousness. See table 2 and figure 3.
Table 2: Secondary Survey
| tracts | findings | actions |
|---|---|---|
| Airway | Clear | |
| Breathing | respiratory rate 18-20/ min, spO2 95% | oxygen is continued until arrival at the hospital |
| Circulation | Sinus rhythm 89/ min (see fig 2) Blood pressure 112/57 mmHg, skin tone is normalizing. | ECG is made |
| Central nervous system |
Maximal EMV-score 15 (4 Eye-opening, 6 best Motor response, 5 best Verbal response) |
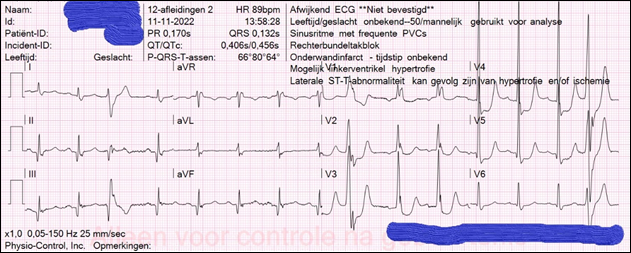
Figure 3: Sinus rhythm 89 beats per minute, electrical axis 80°, PR interval is normal 0.170s, QRS is small, interval 0.132s. some PACs with intraventricular conduction disturbances, ST-segment depression V3, V4, V5
14:02 The patient was transferred to the cardiac care unit of a local hospital in stable condition, arriving at 14:10, following assistance from the ambulance crew and the Advanced Practice Provider (APP). Following a two-day stay in the coronary care unit, the patient’s condition raised concerns of aspiration pneumonia due to oxygen dependency and the development of a fever. Consequently, the patient received antibiotic treatment and was later transferred to the ward. The final phase of treatment involved the placement of an Implantable Cardioverter Defibrillator (ICD) after three weeks.
In the scenario described above, a patient with broad-complex tachycardia was in severe distress and at high risk of requiring resuscitation. In the Netherlands, traditional ambulance crews rely on the Dutch national ambulance protocol when faced with similar cases. The recommended course of action was to administer a Class III antiarrhythmic medication (amiodarone) to the patient and promptly transport them to a hospital. Only if the patient loses consciousness is cardioversion without sedation considered appropriate, although this would likely result in a more challenging situation and possibly a worse prognosis. Sustained VT occurs less frequently, however, accounting for 0.05% of ED visits (Dresen et al., 2018; Domanovits et al., 1999). The acute onset and life-threatening potential of this disorder require accurate and safe management. Therefore, ambulance professionals must be well-trained in the diagnosis and treatment of these patients. In accordance with the 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death, these patients should be treated based on symptoms and etiology. Patients with hemodynamic instability require immediate synchronized cardioversion (Zeppenfeld et al., 2022) which can only be performed under sedation. Therefore, the role of the APP is essential in this situation. All APPs have undergone training similar to emergency physicians, where the training consists of a theoretical part and a practical part, both of which end with an examination. Current guidelines, both national and international, are used for this train¬ing (Richtlijn Sedatie En/Of Analgesie [RSA], 2012; Ambulancezorg Nederland, 2021; Chau et al., 2008; Van Vliet et al., 2024). They are capable of administering sedation to ensure that the patient can be treated in accordance with international guidelines (Ebben et al., 2020; Van vliet, et al., 2024). Medication is titrated until a moderate depth is reached and the patient is in sleep, no longer responds to external stimulation but does retain important reflexes, such as being able to breathe freely, cough and swallow on his/her own. This increases the applicability but also the safety (van Vliet et al., 2024). Although this case describes one patient, one might think that this is a uniquely rare case, however, since implementing the APP and providing sedation in this EMS service, three more patients have been treated with successful emergency cardioversion under sedation (van Vliet, et al., 2022).
The patient remembers the situation well, how lousy he felt, and the feeling that life could be over just like that. After waking up from the sedative, he felt much stronger but he is less socially active and doesn’t dare to do much yet, and slowly he is regaining confidence in his body. Yet he is very grateful for how the ambulance team responded and sees this as a second chance at life.
Although the incidence of such cases is low, the involvement of an APP in managing cardiac arrhythmias can be life-saving, as demonstrated in the case study mentioned. Consequently, we advocate for the implementation of this professional in the Dutch ambulance care.
The patient and all caregivers involved have given their consent to describe this case. All personal information has been anonymized and is not traceable to this patient.
- Ambulancezorg Nederland, (2024). Ambulance Care, Nederland [Internet]. (2024, May 12). Available from: https://www.ambulancezorg.nl/ambulancezorg
- Backus, B. E., Ter Avest, E., Gerretsen, B. M., Viljac, A., & Tolsma, R. T. (2020). Organization of prehospital care in the Netherlands: A perspective article. European Journal of Emergency Medicine, 27(6), 398–9. DOI: https://doi.org/10.1097/mej.0000000000000776
- Ambulancezorg Nederland, (2020). sectoraal kader pilot physician assistant en verpleegkundig specialist ambulancezorg (PAA/VSA).
- van Vliet, R., Deddens, G. J., Evenhuis, R., & Moors, X. R. J. (2022). A survey of the current nurse practitioner and physician assistant workforce in Dutch ambulance care. Int J Nurs Stud Adv, 4. 100099. DOI: https://doi.org/10.1016/j.ijnsa.2022.100099
- Ambulancezorg Nederland, (2016). Landelijk Protocol Ambulancezorg,versie 8.1.
- Dresen, W. F., & Ferguson, J. D. (2018). Ventricular Arrhythmias. Cardiol Clin, 36(1), 129–39. DOI: https://doi.org/10.1016/j.ccl.2017.08.007
- Domanovits, H., Paulis, M., Nikfardjam, M., Holzer, M., Stühlinger, H. G., Hirschl, M. M., & Laggner, A. N. (1999). Sustained ventricular tachycardia in the emergency department. Resuscitation, 42(1), 19–25. DOI: https://doi.org/10.1016/s0300-9572(99)00044-1
- Zeppenfeld, K., Tfelt-Hansen, J., De Riva, M., Winkel, B. G., Behr, E. R., Blom, N. A., Harron, P., Corrado, D., Dagres, N., De Chillou, C., Eckardt, L., Friede, T., Haugaa, K. H., Hocini, M., Lambiase, P. D., Marijon, E., Merino, J. L., Peichl, P., Priori, S. G., Reichlin, T., Schulz-Menger, J., Sticherling, C., Tzeis, S., Verstrael, A., Volterrani, M., & ESC Scientific Document Group (2022). ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: Developed by the task force for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur Heart J, 43(40), 3997–4126. DOI: https://doi.org/10.1093/eurheartj/ehac262
- Richtlijn Sedatie En/Of Analgesie (RSA), (2012). OP LOCATIES BUITEN DE OPERATIEKAMER – PDF Free Download [Internet]. [2022, Nov 28]. Available from: https://docplayer.nl/55230354-Richtlijn-sedatie-en-of-analgesie-psa-op-locaties-buiten-de-operatiekamer.html
- Ambulancezorg Nederland, (2021). Sectorkompas Ambulancezorg 2020. (september):104. Available from: https://www.ambulancezorg.nl/sectorkompas/sectorkompas-2020
- Chau, D. L., Walker, V., Pai, L., & Cho, L. M. (2008). Opiates and elderly: Use and side effects. Clin Interv Aging, 3(2), 273–8.
DOI: https://doi.org/10.2147/cia.s1847 - van Vliet, R., Breedveld, L., Heutinck, A. A. J., Ockeloen, B. H. A,, van ’ Hof, A. W. J., & Moors, X. R. J. (2024). Procedural sedation by advanced practice providers in the emergency medical service in the Netherlands: a retrospective study. Scand J Trauma Resusc Emerg Med, 32(1).
DOI: https://doi.org/10.1186/s13049-024-01207-z - Ebben, R., Vliet van, R., Breedveld, L., Douwes, I., Hereijgers, J., Pas van de, H., & Vloet, L. C. M. (2020). Implementation of a Nurse Practitioner in Emergency Ambulance Care in the Netherlands: A Study Protocol for the IMPACT-Study. Researchgate. https://www.researchgate.net/publication/346339867_Implementation_of_A_Nurse_Practitioner_in_Emergency_Ambulance_Care_in_The_Netherlands_A_Study_Protocol_for_The_IMPACT-Study.













