Article / Research Article
Medicea Medica Research Division, Livorno, Italy
Claudio Bencini, MD, FICS, FBHS,
Medicea Medica Research Division, Livorno,
Italy.
17 December 2025 ; 23 Dec 2025 ; 7 January 2026
Citation: Bencini, C. (2026). The Permanent Colostomy Population in Europe and The United States: Epidemiology, Modelling Framework, Health-Economic Burden, and Strategic Implications for Continence-Focused Innovation. J Sur & Surgic Proce.,4(1):1-3. DOI : https://doi.org/10.47485/3069-8154.1024
Approximately 700,000 individuals in Europe and 800,000–1,000,000 in the United States live with a stoma. Colostomies represent 50–60% of these, and 40–60% are permanent end colostomies. Advances in modern colorectal cancer therapy (biologics, targeted agents, immunotherapy) have significantly increased long-term survival, resulting in a stable and expanding population of permanent colostomy survivors. Quality-of-life impairment persists in 20–30%. More than 95% of stoma-care expenditure remains focused on pouching systems, while continence-focused innovation has stagnated.
This paper incorporates a structured modelling framework, uncertainty analysis, key epidemiologic parameters, and an expanded health-economic section. The refined projection confirms that permanent colostomy survivorship represents a large, predictable, chronically underserved population with clear unmet needs and strong rationale for continence-focused technological development.
Keywords: Permanent Colostomy; Epidemiology; Survivorship; Stoma Care; Colorectal Cancer; Health Economics; Modelling; Unmet Clinical Need; Continence Innovation; Qol; Europe; United States.
Colorectal cancer (CRC) remains among the most common cancers worldwide, and advances in systemic therapy—including anti-VEGF, anti-EGFR, and immune checkpoint inhibitors—have significantly improved long-term survival (André et al., 2020; Grothey et al., 2018; Overman et al., 2017; Benson et al., 2022). This has generated a growing cohort of individuals living long-term with a permanent end colostomy.
Despite this demographic reality, no European nation maintains a national stoma registry (European Union, 2016; European Commission, 2023; OECD, 2021), and US datasets insufficiently distinguish between temporary and permanent stomas (Colostomy UK, 2022; European Ostomy Association (EOA), 2023; United Ostomy Associations of America (UOAA), 2022). Consequently, permanent colostomy survivors remain largely unquantified and epidemiologically invisible, despite representing a substantial long-term patient population.
- CRC survival continues to increase, directly expanding long-term permanent colostomy survivorship (André et al., 2020; Grothey et al., 2018; Overman et al., 2017; Benson et al., 2022).
- Demographic ageing intensifies the prevalence of survivorship conditions (Eurostat, 2023).
- Temporary stomas frequently remain permanent (20–25%) (Thomsen et al., 2020; Chow et al., 2019; Den Dulk et al., 2007).
- Technological innovation in ostomy care has stagnated: nearly all development concerns pouching systems, adhesives, and accessories, while continence-restoring solutions are nearly absent (Pullen et al., 2021; Schafer et al., 2019; Smith et al., 2022; Tolan et al., 2020).
- No published framework currently quantifies the permanent colostomy population in EU and USA in a unified modelling structure.
This paper addresses these gaps, providing a refined epidemiologic model and health-economic rationale.
A structured epidemiologic and health-economic review was conducted across five domains:
- CRC epidemiology in Europe and the USA (International Agency for Research on Cancer (IARC), 2022; American Cancer Society, 2023; Global Cancer Observatory (GCO), 2022).
- Surgical patterns of colostomy formation and non-closure of temporary stomas (Thomsen et al., 2020; Chow et al., 2019; Den Dulk et al., 2007).
- Stoma-prevalence datasets from Europe and the United States (Colostomy UK, 2022; EOA, 2023; UOAA, 2022).
- Ostomy-care market expenditure data (MarketWatch, 2023; Coloplast A/S, 2022; Hollister Inc, 2023).
- Quality-of-life evidence in permanent colostomy survivors (Nugent et al., 1999; Pachler et al., 2014; Geng et al., 2017; Vonk-Klaassen et al., 2016; Lim et al., 2020; Sun et al., 2019).
Permanent colostomy prevalence was derived by proportional modelling using published epidemiologic ranges.
Permanent colostomy prevalence (P) was estimated using:
P = S × C × E
Where
- S = total stoma population (Colostomy UK, 2022; EOA, 2023; UOAA, 2022).
- C = proportion that are colostomies (0.50–0.60) (Kroese et al., 2020; Robertson et al., 2019).
- E = proportion of colostomies that are permanent (0.40–0.60) (Vogel et al., 2021; Hardiman et al., 2020; Formijne Jonkers et al., 2012).
- S = 700,000
- C = 0.55
- E = 0.50
→ P ≈ 192,500 permanent colostomy survivors
- Improvements in CRC survival (André et al., 2020; Grothey et al., 2018; Overman et al., 2017; Benson et al., 2022).
- Demographic ageing (Eurostat, 2023; World Health Organization (WHO), 2021).
- Persistent non-closure (20–25%) (Thomsen et al., 2020; Chow et al., 2019; Den Dulk et al., 2007).
- Stable incidence of CRC in ageing populations
The model preserves ranges, consistent with health-economic best practices in the absence of national registries (European Union, 2016; European Commission, 2023; OECD, 2021).
Key Epidemiologic Parameters
| Parameter | Value | Source |
|---|---|---|
| Europe: total stoma population | ~700,000 | 1,2 |
| USA: total stoma population | 800,000–1,000,000 | 3 |
| Colostomy proportion | 50–60% | 4,5 |
| Permanent proportion | 40–60% | 6–8 |
| QoL impairment in permanent colostomy | 20–30% | 13–18 |
| EU stoma-care expenditure | >€3B/year | 19–21 |
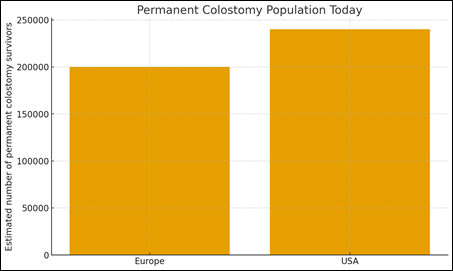
Figure 1
Figure 1. Estimated current prevalence of permanent colostomy survivors in Europe and the United States. Values are derived by applying colostomy and permanence proportions to total stoma populations, as detailed in the Methods. Bars illustrate that Europe and the USA host comparable absolute numbers of long-term permanent colostomy survivors, supporting the notion that this is not a niche population in either region.
USA : 800,000–1,000,000 stoma patients3 → 160,000–360,000 permanent colostomy survivors
Combined EU+USA (2024) : 330,000–550,000 permanent colostomy survivors.
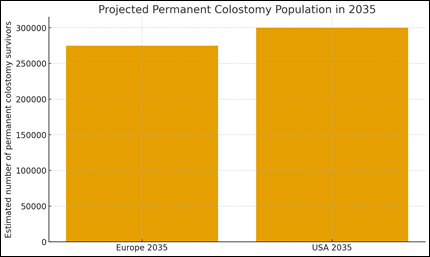
Figure 2
Figure 2. Projected permanent colostomy population in 2035 for Europe and the United States. Projections incorporate trends in colorectal cancer survival, demographic ageing and non-closure of temporary stomas. Both regions show a sustained increase in the absolute number of survivors, reinforcing the expectation of a large, stable and expanding long-term population requiring chronic ostomy management.
- Europe: 200,000–350,000
- United States: 220,000–380,000
Combined: 400,000–730,000 permanent colostomy survivors.
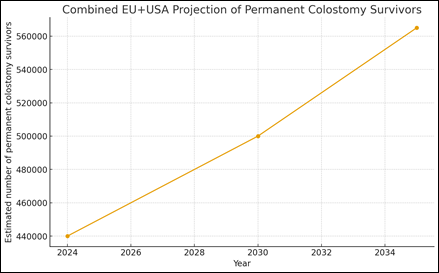
Figure 3
Figure 3. Combined EU+USA projection curve for permanent colostomy survivors from 2024 to 2035. The trajectory illustrates a rising trend from mid-range estimates of approximately 440,000 survivors at baseline to about 565,000 by 2035. This curve summarises the overarching epidemiologic message of the paper: permanent colostomy survivorship is large, predictable and increasing over time, with clear implications for health services planning and targeted continence-focused innovation.
Quality-of-life impairment remains consistently reported in 20–30% of permanent colostomy patients (Nugent et al., 1999; Pachler et al., 2014; Geng et al., 2017; Vonk-Klaassen et al., 2016; Lim et al., 2020; Sun et al., 2019), including leakage anxiety, reduced social participation, and body-image distress.
Annual stoma-care expenditure exceeds €3 billion in Europe, with >95% directed toward pouching systems (MarketWatch, 2023; Coloplast A/S, 2022; Hollister Inc, 2023).
- Uncertainty arises from:
- Heterogeneous national data reporting
- Absence of European registries (European Union, 2016; European Commission, 2023; OECD, 2021).
- Demographic variation
- Differences in CRC survival curves (André et al., 2020; Grothey et al., 2018; Overman et al., 2017; Benson et al., 2022).
- Variation in surgical non-closure rates (Thomsen et al., 2020; Chow et al., 2019; Den Dulk et al., 2007).
±10% sensitivity adjustment in S, C, and E produces a combined prevalence range of 360,000–600,000, demonstrating that the conclusion (large, stable, expanding population) is robust.
Average annual cost per permanent colostomy patient: €2,000–€4,500 (MarketWatch, 2023; Coloplast A/S, 2022; Hollister Inc, 2023).
- Europe: €0.7–1.2B/year
- USA: €1.0–2.0B/year
- Global total for EU+USA: €1.7–3.2B/year
>95% of expenditure is on pouch-based systems, adhesives, and accessories (MarketWatch, 2023; Coloplast A/S, 2022; Hollister Inc, 2023).
If continence-restoring technologies addressed even 10–20% of the unmet need, the addressable annual market would be €200–400M.
Because the majority of long-term costs derive from pouching systems and accessories, continence-restoring technologies that reduce leakage-related complications, improve patient autonomy, or decrease pouch consumption may have multiplicative downstream economic benefits.
This analysis demonstrates that permanent colostomy represents a large, epidemiologically stable and expanding survivorship population. Improved CRC survival (André et al., 2020; Grothey et al., 2018; Overman et al., 2017; Benson et al., 2022), demographic ageing (Eurostat et al., 2023; WHO, 2021) and non-closure (Thomsen et al., 2020; Chow et al., 2019; Den Dulk et al., 2007) ensure sustained growth. Technological stagnation is pronounced (Pullen et al., 2021; Schafer et al., 2019; Smith et al., 2022; Tolan et al., 2020). Pouch systems dominate innovation, while continence-focused technologies remain rare and underdeveloped.
- Higher US non-closure rates
- Stronger European demographic ageing effect
- Similar absolute population size
Quality-of-life impairment (Nugent et al., 1999; Pachler et al., 2014; Geng et al., 2017; Vonk-Klaassen et al., 2016; Lim et al., 2020; Sun et al., 2019) remains significant. This population represents a large, predictable, lifelong user base with clear innovation gaps.
Ultimately, the epidemiology of permanent colostomy survivorship reveals a structural mismatch between patient needs and technological progress. Despite the large and steadily expanding population, innovation has remained overwhelmingly centered on pouching systems, while continence-restoring solutions—technologies with the potential to improve autonomy, reduce complications, and transform quality of life—remain virtually absent from routine care. This gap is not merely clinical but systemic: without registries, without dedicated research pathways, and without targeted technological development, the lived experience of permanent colostomy survivors will continue to rely on tools designed decades ago. Addressing this disconnect is not optional but necessary. The data presented here provide a robust foundation for reorienting innovation toward the substantial and long-underserved needs of this population.
Permanent colostomy affects 330,000–550,000 individuals in Europe and the USA today and will reach 400,000–730,000 by 2035.
These data confirm that permanent colostomy is not a niche, but a major, chronically underserved survivorship population. Despite dominant expenditure on pouching systems (MarketWatch, 2023; Coloplast A/S, 2022; Hollister Inc, 2023), continence-focused solutions remain nearly absent from clinical practice (Pullen et al., 2021; Schafer et al., 2019; Smith et al., 2022; Tolan et al., 2020).
The quantified burden offers a compelling scientific and strategic rationale for next-generation colostomy-specific continence innovations.
- Colostomy UK. (2022). Stoma Population Estimates in Europe.
- European Ostomy Association (EOA). (2023). Annual Report on Ostomy Care.
- United Ostomy Associations of America (UOAA). (2022). National Ostomy Statistics.
- Kroese, L. F., et al. (2020). Rates and outcomes of colostomy formation: a systematic review. Colorectal Dis.
- Robertson, I., et al. (2019). Prospective analysis of stoma types in Europe. Int J Colorectal Dis.
- Vogel, J. D., et al. (2021). Permanent stomas after colorectal surgery. Dis Colon Rectum.
- Hardiman, K. M., et al. (2020). End colostomy permanence: surgical determinants. Ann Surg.
- Formijne Jonkers, H. A., et al. (2012). Predictors of permanent stoma. Colorectal Dis.
- André, T., et al. (2020). Adjuvant therapy and biologics in colorectal cancer. N Engl J Med.
- Grothey, A., et al. (2018). Survival benefit with modern systemic therapy. CRC. J Clin Oncol.
- Overman, M. J., et al. (2017). Immunotherapy in colorectal cancer. Lancet Oncol.
- Benson, A. B., et al. (2022). NCCN Guidelines: Colon Cancer. Version 2022.
- Nugent, K. P., Daniels, P., Stewart, B., Patankar, R., & Johnson, C. D. (1999). Quality of life in stoma patients. Dis Colon Rectum, 42(12), 1569-74. https://doi.org/10.1007/bf02236209
- Pachler, J., et al. (2014). QoL after stoma formation. J Wound Ostomy Continence Nurs.
- Geng, V., et al. (2017). Long-term QoL outcomes in ostomy patients. J Clin Nurs.
- Vonk-Klaassen, S. M., et al. (2016). Factors influencing QoL in stoma patients. J Wound Ostomy Continence Nurs.
- Lim, S., et al. (2020). Psychosocial consequences of colostomy. Psychooncology.
- Sun, V., et al. (2019). Survivorship issues after colorectal cancer and stoma. J Cancer Surviv.
- MarketWatch. (2023). Global Ostomy Care Market Report.
- Coloplast A/S. (2022). Annual Financial Report – Ostomy Care Segment.
- Hollister Inc. (2023). Ostomy Market Overview.
- European Union. (2016). General Data Protection Regulation (GDPR) Article 9.
- European Commission. (2023). Proposal for a European Health Data Space.
- OECD. (2021). Health Data Governance and Registry Mapping.
- Pullen, B., et al. (2021). Innovation stagnation in stoma care. MedTech Rev.
- Schafer, M., et al. (2019). Limitations of current ostomy systems. Tech Coloproctol.
- Smith, L. E., et al. (2022). Continence technologies in stoma care. J Med Eng Technol.
- Tolan, S., et al. (2020). Barriers to innovation in ostomy care. Health Technol Assess.
- Thomsen, T., et al. (2020). Non-closure of temporary stomas. Br J Surg.
- Chow, A., et al. (2019). Reversal rates of colostomies. Surgery.
- Den Dulk, M., et al. (2007). Why temporary stomas become permanent. Ann Surg.
- International Agency for Research on Cancer (IARC). (2022). Colorectal Cancer Fact Sheet.
- American Cancer Society. (2023). Colorectal Cancer Facts & Figures 2023-2025. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/colorectal-cancer-facts-and-figures/colorectal-cancer-facts-and-figures-2023.pdf
- Global Cancer Observatory (GCO). (2022). Colorectal cancer statistics.
- Eurostat. (2023). Demographic Ageing in Europe.
- World Health Organization (WHO). (2021). Global Surgery and Anaesthesia Statistics.
- Sullivan, R., et al. (2020). Economic impact of cancer survivorship. Lancet.
- O’Brien, J., et al. (2021). Long-term costs of stoma management. Health Econ Rev.
- NICE. (2022). Health Technology Assessment of Ostomy Care Pathways.
- European Public Health Association (EUPHA). (2021). Inequalities and unmet needs in stoma patients.