Article / Case Report
Department of Cardiology, Traditional Chinese Medicine Hospital of Kunshan, Suzhou, Jiangsu 215300, China.
Dr. Wen Pan
Department of Cardiology,
Traditional Chinese Medicine Hospital of Kunshan, Suzhou,
Jiangsu 215300,
China.
14 September 2023 ; 2 October 2023
Wolf-Parkinson-White (WPW) syndrome with atrial fibrillation (AF) may be life threatening and catheter ablation is the top priority choice. Accessory pathways (APs) in this patient may locate in the posterior septum. We present a successful case of WPW with AF, which we ablated inside the middle cardiac vein (MCV).
The report describes a case of WPW syndrome that was ablated within the MCV. A 42 male was referred to our hospital for palpitation and hypotension. After electrical cardioversion, a 12-lead electrocardiogram (ECG) in sinus rhythm showed preexcitation indicating a posteroseptal AP. Ablation in the right posterior septum of the endocardium could not completely block the conduction of AP and the best target site was mapped within MCV. The successful ablation sites were confirmed in MCV by angiography and AF never appeared during follow-up.
When ablation of the posterior septum for APs from an endocardial approach has failed, venography should be performed to assess CS anatomy and mapping should be performed within the CS and its major branches. In young patients with AF and preexcitation, ablation of APs can prevent AF.
Wolf-Parkinson -White syndrome; atrial fibrillation; middle cardiac vein; radiofrequency ablation
Patients having Wolf-Parkinson-White (WPW) and atrial fibrillation (AF) have a higher association of posteriorly and epicardial accessory pathways (APs). Ablation is the top priority choice for patients with AF and WPW because rapid anterograde conduction through the accessory pathway may induce ventricular fibrillation and potentially sudden cardiac death (Bazoukis et al., 2022). Posterosetal APs are difficult to ablate because the myocardial coat comprises 36% of posterosetal Aps (Sun et al., 2002). Epicardial APs should be completely blocked through the epicardial approach owing to the extensive connections. We present a successful case of WPW with AF, which we ablated inside the middle cardiac vein (MCV).
A 42-year-old man was referred to our hospital with palpitations and hypotension. The electrocardiogram (ECG) during tachycardia demonstrated a fast irregular wide QRS tachycardia. The ventricular rate was > 200/minute with the shortest RR interval of 200 msec (Fig.1A). Electrical cardioversion successfully restored sinus rhythm. Tachycardia converted to sinus rhythm after electrical cardioversion. ECG in sinus rhythm showed a wide QRS complex, short PR interval, and delta wave (Fig.1B).The delta wave morphology indicates a right posteroseptal AP. The physical examination,blood chemistry data and echocardiogram were normal on admission.
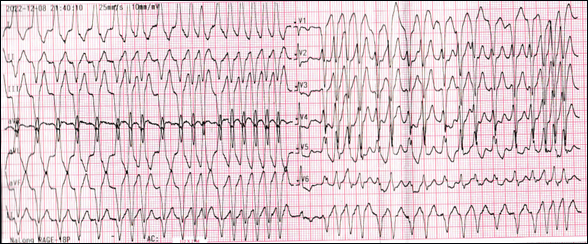 Figure 1 (A): ECG shows fast irregular wide polymorphic QRS complex tachycardia. The shortest RR interval is 200 msec.
Figure 1 (A): ECG shows fast irregular wide polymorphic QRS complex tachycardia. The shortest RR interval is 200 msec.
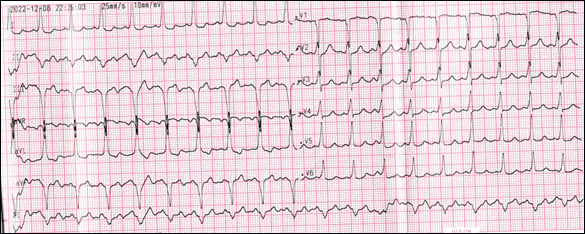 Figure 1 (B): ECG after cardioversion shows sinus rhythm with wide QRS complex, short PR interval, and delta wave suggesting a posteroseptal accessory pathway.
Figure 1 (B): ECG after cardioversion shows sinus rhythm with wide QRS complex, short PR interval, and delta wave suggesting a posteroseptal accessory pathway.
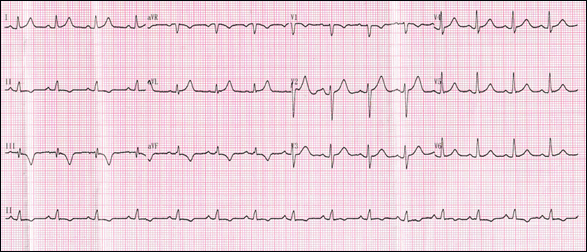 Figure 1 (C): ECG after RFA shows sinus rhythm with narrow QRS complex,normal PR interval, and without delta wave.
Figure 1 (C): ECG after RFA shows sinus rhythm with narrow QRS complex,normal PR interval, and without delta wave.
Figure 1 : ECG in a patient with WPW syndrome during AF and sinus rhythm before and after RFA.
Written informed consent was obtained and an electrophysiological (EP) study was performed. A decapolar catheter was advanced into the coronary sinus (CS) and a quadripolar catheter was positioned into the right ventricular apex through the right femoral vein. A 3.5-mm, externally irrigated radiofrequency catheter (Biosense Webster, Diamond Bar, CA, USA) was advanced. Fusion of atrial and ventricular potentials with the earliest ventricular activation was recorded in the right posteroseptal region. Radiofrequency ablation (RFA) was performed in the right posterior septum through an endocardial approach and preexcitation disappeared at 10 seconds of application (Fig.2A) but the retrograde of AP always existed after several ablations (Fig.2B).
 Figure 2(A): Abrupt disappearance of delta wave and the dissociation between the two potentials after successful ablation (bottom arrow) . Paper speed is 100 mm/s.
Figure 2(A): Abrupt disappearance of delta wave and the dissociation between the two potentials after successful ablation (bottom arrow) . Paper speed is 100 mm/s.
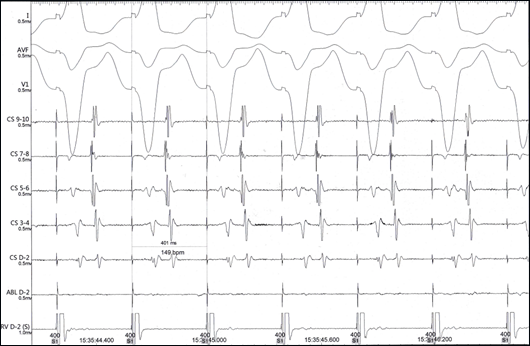 Figure 2(B): Retrograde Conduction of Accessory Pathway always exited with right ventricular apical pacing at the cycle length of 400ms after ablation through endocardial approach.Paper speed is 100 mm/s.
Figure 2(B): Retrograde Conduction of Accessory Pathway always exited with right ventricular apical pacing at the cycle length of 400ms after ablation through endocardial approach.Paper speed is 100 mm/s.
Catheter was extended into the CS and the earliest atrial activity with a stable VA interval, which was 22 ms earlier than the ostium of CS (Fig.2C), was detected approximately 1 cm inside the MCV. RF energy was delivered with an initial power of 25W, up-titrated to a maximum power of 30W with an irrigation rate of 30mL/min for almost 90 seconds while carefully monitoring impedence,temperature, degree of chest pain and ECG. Ventriculoatrial conduction was dissociated with pacing at the cycle length of 500ms (Fig.2D).Repeated electrical stimulation was performed, antegrade and retrograde conduction of AP and AF were not observed even with isoprenaline infusion. ECG after RFA showed normal sinus rhythm with a narrow QRS complex, normal PR interval, and without delta wave (Fig.1C). Injection of contrast through RF catheter proved that the target site was in the MCV (Fig.3).There were no procedure-related complications and the patient remained well and asymptomatic during six months of follow up without any evidence of delta wave and AF in repeated ECGs.
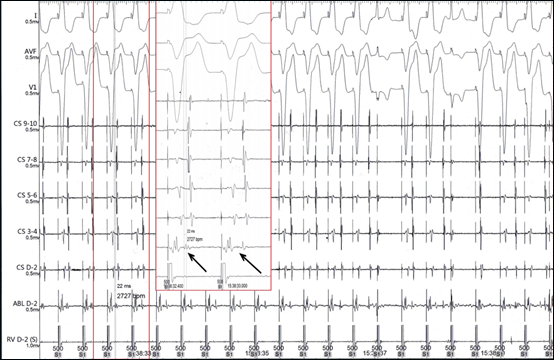 Figure 2(C): Catheter was extended into the coronary sinus and the earliest atrial activity with a stable VA interval, which was 22 ms earlier than the ostium of coronary sinus.Ventriculoatrial conduction was dissociated with pacing at the cycle length of 500ms about ten seconds after ablation.Paper speed is 25mm/s
Figure 2(C): Catheter was extended into the coronary sinus and the earliest atrial activity with a stable VA interval, which was 22 ms earlier than the ostium of coronary sinus.Ventriculoatrial conduction was dissociated with pacing at the cycle length of 500ms about ten seconds after ablation.Paper speed is 25mm/s
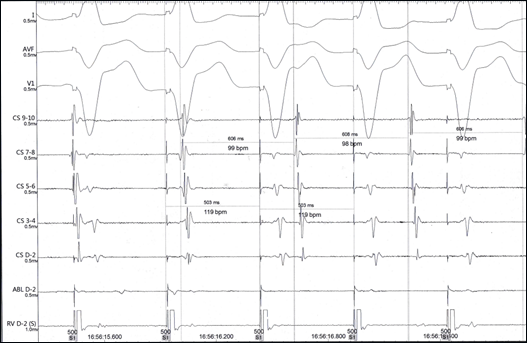 Figure 2(D): Ventriculoatrial conduction was dissociated with pacing at the cycle length of 500ms.Paper speed is 100 mm/s. CS D-2, distal coronary sinus; CS9-10, proximal coronary sinus; RV, right ventricle; CS, coronary sinus;ABL, ablation.
Figure 2(D): Ventriculoatrial conduction was dissociated with pacing at the cycle length of 500ms.Paper speed is 100 mm/s. CS D-2, distal coronary sinus; CS9-10, proximal coronary sinus; RV, right ventricle; CS, coronary sinus;ABL, ablation.
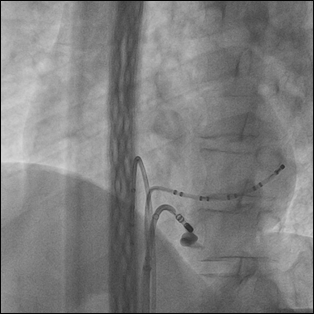 Figure 3(A): Left Anterior Oblique(LAO)
Figure 3(A): Left Anterior Oblique(LAO)
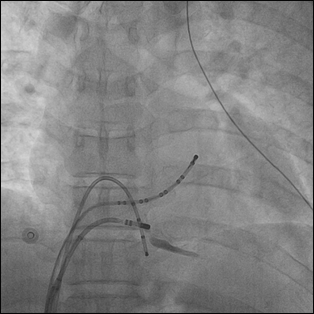 Figure 3(B): anteroposterior(AP)
Figure 3(B): anteroposterior(AP)
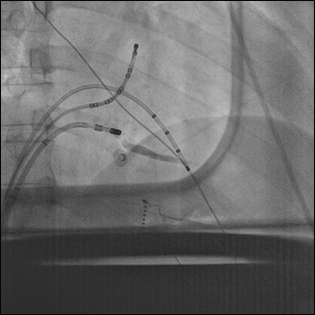 Figure 3(C): The tip of the ablation catheter at the successful ablation site was located in proximal MCV.
Figure 3(C): The tip of the ablation catheter at the successful ablation site was located in proximal MCV.
WPW syndrome with AF may be life threatening because of excessive ventricular response. For such patients, APs often locate in the posterior septum and blocking the APs is the most effective method (Acharya et al., 2020). Extension of the CS venosus muscle may connect the atrium and ventricle in pathology studies.Because of the wide connection of posterior septal AP, venography should be performed to assess CS anatomy and mapping should be performed within the CS and its major branches if endocardial ablation in the posterior septum fails.
(Tebbenjohanns et al., 1996) have conducted direct CS angiography in 23 patients with posteroseptal APs. A CS diverticulum was found in 6 (26%), MCV in 6 (26%), and 2 (6%) patients had a vein draining into the proximal part of the CS. Successful RF application was attempted within the CS in 11 (48%) of 23 patients.
Ablation within the coronary veins can easily lead to serious complications, such as cardiac tamponade, coronary artery injury, AV block, and coronary sinus thrombosis. These risks can be minimized with proper adjustment of the RF generator settings and appropriate ablation catheter. In our experience, an irrigated catheter is preferred and the catheter must point towards the ventricle by maintaining a subtle counterclockwise torque. During ablation, A low energy (20-30 W) is recommended and attention must be paid to impedence,temperature, degree of chest pain and ECG.
After successful ablation of AP, AF was not induced and on follow-up AF never appeared again. In a study by Dagres et al. (Dagres et al., 2001), such patients with more than 50 years had a higher incidence of AF on follow-up. In this case,the patient was much younger and therefore ablation of APs is enough. If new onset of AF was recorded on follow-up, circumferential pulmonary vein isolation should be done (Cui et al., 2022).
RFA in young patients with WPW and AF has good clinical outcomes. When ablation of the posterior septum for APs from an endocardial approach has failed, venography should be performed to assess CS anatomy and mapping should be performed within the CS and its major branches. An irrigated catheter and low energy are recommended when ablation in CS is required. In young patients with AF and preexcitation, ablation of APs can prevent AF.
The authors declare no conflict of interest.
- Bazoukis, G., Papasavvas, E., Pavlou, M., Georgiou, P., Kapetis, L., Patestos, D., Vlachos, K., Saplaouras, A., Letsas, K. P., Efremidis, M., & Tsielepis, M. (2022). Atrial fibrillation and Wolff-Parkinson-White syndrome: A double blow for the cardiologist. Clinical case reports, 10(7), e6035.
DOI:https://doi.org/10.1002/ccr3.6035 - Sun, Y., Arruda, M., Otomo, K., Beckman, K., Nakagawa, H., Calame, J., Po, S., Spector, P., Lustgarten, D., Herring, L., Lazzara, R., & Jackman, W. (2002). Coronary sinus-ventricular accessory connections producing posteroseptal and left posterior accessory pathways: incidence and electrophysiological identification. Circulation, 106(1), 1362-1367. DOI: https://doi.org/10.1161/01.cir.0000028464.12047.a6
- Acharya, D., Rane, S., Bohora, S., & Kevadiya, H. (2020). Incidence, clinical, electrophysiological characteristics and outcomes of patients with Wolff-Parkinson-White syndrome and atrial fibrillation. Indian pacing and electrophysiology journal, 20(1), 3-7.
DOI: https://doi.org/10.1016/j.ipej.2019.12.015 - Tebbenjohanns, J., Pfeiffer, D., Schumacher, B., Jung, W., Manz, M., & Lüderitz, B. (1996). Direct angiography of the coronary sinus: impact on left posteroseptal accessory pathway ablation. Pacing and clinical electrophysiology, PACE, 19(7), 1075-1081. DOI: https://doi.org/10.1111/j.1540-8159.1996.tb03416.x
- Dagres, N., Clague, J. R., Lottkamp, H., Hindricks, G., Breithardt, G., & Borggrefe, M. (2001). Impact of radiofrequency catheter ablation of accessory pathways on the frequency of atrial fibrillation during long-term follow-up; high recurrence rate of atrial fibrillation in patients older than 50 years of age. European heart journal, 22(5), 423-427. DOI : https://doi.org/10.1053/euhj.2000.2429
- Cui, C., Li, Z., Ju, W., Yang, G., Gu, K., Liu, H., Li, M., Chen, H., Wang, J., & Chen, M. (2022). The characteristics of pre-excitation syndrome concomitant with atrial tachyarrhythmia and the effect of radiofrequency ablation. Pacing Clin Electrophysiol, 45(12), 1401-1408. DOI:https://doi.org/10.1111/pace.14598













