Article / Case Report
1Heart and Vascular Institute Henry Ford West Bloomfield Hospital, West Bloomfield, MI
2Heart and Vascular Institute, Henry Ford Hospital, Detroit, MI
3Detroit Country Day School, Beverly Hills, MI
4Dept of Cardiology, Henry Ford Macomb Hospital, Clinton Township, MI
5Dept of Cardiology, Henry Ford Macomb Hospital, Clinton Township, MI
6Dept of Cardiology, Henry Ford Macomb Hospital, Clinton Township, MI
Karthik Ananthasubramaniam, MD FACCMD FACC FASE FASNC FSCCT FSCMR FRCP
Henry Ford West Bloomfield Hospital,
Heart and Vascular Institute
6777 West Maple
West Bloomfield MI
USA 48322
17 August 2021 ; 1 September 2021
Keywords: Spindle Cell Sarcoma; Pulmonary Stenosis; Supravalvular Pulmonic Stenosis; Histopathology; Echocardiography; Computed Tomography; Magnetic Resonance Imaging.
Pulmonary artery malignancies are extremely rare, with a reported occurrence of 0.001-0.03% and almost all being sarcomas from the intima and worldwide less than 250 cases have been reported [1, 2]. A high degree of suspicion is required to diagnose this tumor as imaging modalities may not adequately identify this tumor [1-3] posing challenges in diagnosis as illustrated in our case. Because of the high mortality associated with this malignancy, early and aggressive intervention is crucial.
We present a case of a 59-year-old female with a history of hypothyroidism who presented with progressive exertional dyspnea and palpitations. She underwent a contrast chest computed tomography scan (CT) for suspected pulmonary embolism which was negative but revealed diffuse long tubular narrowing above the pulmonary valve involving the main pulmonary artery (MPA) and raising suspicion for supravalvular pulmonic stenosis (SPS) (Figure 1).

Figure 1: Contrast enhanced chest CT showing diffuse supravalvular narrowing and no obvious extrinsic compression of pulmonary artery.
A two dimensional echocardiogram revealed normal left and right ventricular function as well as elevated systolic velocities distal to the pulmonic valve with a peak gradient of 37 mm hg suggestive of SPS (Figure 2a and 2b).
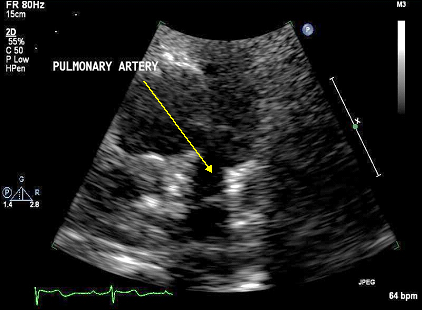
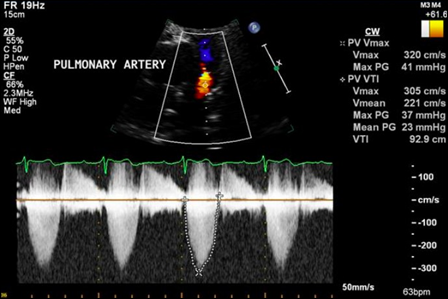
Figures 2a and 2b: Transthoracic echocardiogram revealing normal pulmonary valve and diffuse supravalvular narrowing (top image) with doppler images showing elevated velocities and gradients across pulmonic valve (bottom image).
A non-contrast cardiac magnetic resonance imaging (MRI) was performed to evaluate for congenital disease and SPS confirming narrowing of the main pulmonary artery 1 cm distal to a normal appearing pulmonic valve, with the narrowest area measuring 9mm in diameter (Figure 3).
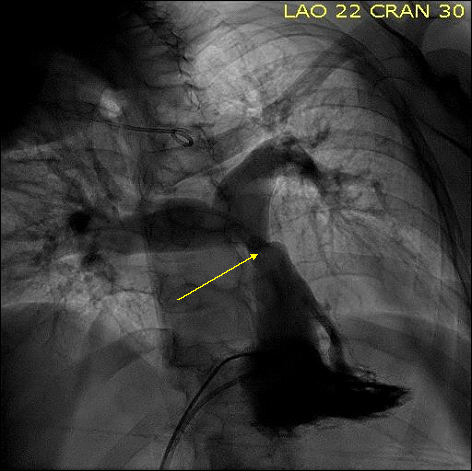 Figure 3: Right ventricular and PA angiogram showing diffuse supravalvular pulmonary artery narrowing.
Figure 3: Right ventricular and PA angiogram showing diffuse supravalvular pulmonary artery narrowing.
The patient underwent a cardiac catheterization and a right ventricular and pulmonary artery angiogram (Figure 4) which demonstrated a peak gradient of 67 mm Hg across the stenotic lesion in the MPA. She was then diagnosed as symptomatic congenital isolated SPS.
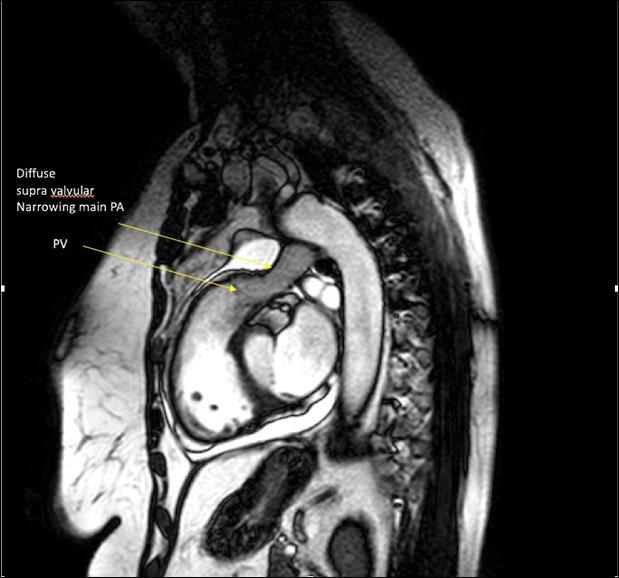 Figure 4: Steady state free precession (SSFP) cine still image of RV outflow tract showing pulmonic valve (PV) and diffuse supravalvular narrowing of main PA.
Figure 4: Steady state free precession (SSFP) cine still image of RV outflow tract showing pulmonic valve (PV) and diffuse supravalvular narrowing of main PA.
Intraoperatively, a segment of the pulmonary artery was noted to be circumferentially narrowed by an extrinsic infiltrative process. Frozen section analysis confirmed sarcoma, possible spindle cell variant. The MPA was resected to the level of the pulmonary artery bifurcation and the tumor was debulked (Figure 5) and a 23 mm aortic homograft was sewed in place.

Figure 5: Gross operative specimen of leiomyosarcoma.
On final pathology, the tumor was diagnosed as a high-grade spindle cell sarcoma. The cells were negative for MDM2 gene amplification by fluorescence in-situ hybridization. Although the sarcoma had some morphologic features suggestive of smooth muscle differentiation, the lack of caldesmon or desmin staining precluded more definitive classification of this tumor. (Figure 6A-D). A re-review of the CT and MRI failed to conclusively predict the presence of this encircling tumor around the pulmonary artery. Following surgery and recovery, the patient underwent a positron emission tomography (PET) scan which demonstrated a small lytic lesion at L1, with a possible metastatic femoral neck lesion. She was seen by hematology/oncology with recommendations to undergo localized radiotherapy and chemotherapy. The patient delayed treatment for her sarcoma in anticipation of a second opinion, and she ultimately passed away.
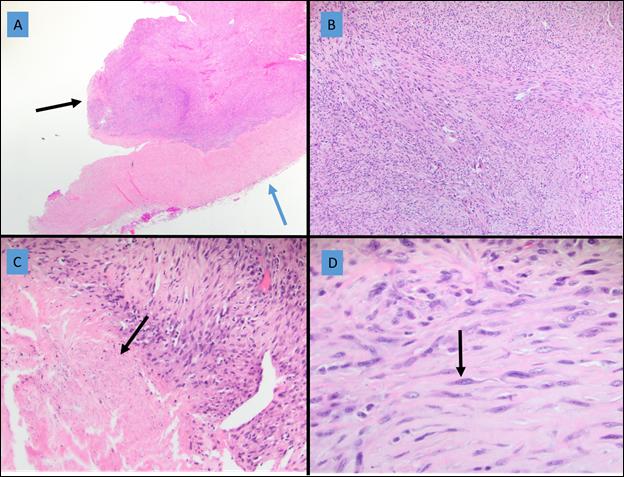 Figure 6: A, High-grade spindle-cell sarcoma (black arrow) is seen adjacent to fibrous tissue (blue arrow). B, The tumor cells exhibit a fascicular architecture. C, Cellular necrosis is identified (black arrow). D, Higher magnification shows the spindled cells to contain focal areas of nuclei with blunt ends (black arrow). While the fascicular architecture and blunted nuclei might suggest smooth muscle differentiation, the lack of definitive immunohistochemical staining precludes more definitive classification beyond high-grade spindle cell sarcoma.
Figure 6: A, High-grade spindle-cell sarcoma (black arrow) is seen adjacent to fibrous tissue (blue arrow). B, The tumor cells exhibit a fascicular architecture. C, Cellular necrosis is identified (black arrow). D, Higher magnification shows the spindled cells to contain focal areas of nuclei with blunt ends (black arrow). While the fascicular architecture and blunted nuclei might suggest smooth muscle differentiation, the lack of definitive immunohistochemical staining precludes more definitive classification beyond high-grade spindle cell sarcoma.
High grade sarcomas arising from the MPA are extremely rare and pose major diagnostic challenges and sometimes manifests as a filling defect involving the pulmonary artery mimicking a pulmonary embolism [1]. A case of similar nature to ours was described in 2017 presenting as adult onset pulmonic stenosis and ultimately diagnosed as spindle cell sarcoma [2]. Leiomyosarcoma of pulmonary artery has also manifested similarly masquerading as other pathology. Although some tumor features in our case suggested a leiomyosarcoma, definitive diagnostic criteria was not present to differentiate beyond spindle cell sarcoma. In our case, multiple imaging studies were performed including a CT, MR, and TTE, all of which failed to conclusively reveal the extrinsic circumferential compression of the main pulmonary artery. As illustrated in prior reports [3] even advanced imaging studies miss pulmonary artery malignancies presurgically leading to misdiagnosis and definitive diagnosis is sometimes only with immunohistopathology. Hence in patients who do not have other congenital anomalies, isolated narrowing of the MPA presenting as adult pulmonic or supravalvular stenosis should be approached with a high degree of suspicion to rule out extrinsic compression by a tumor, as was evident in our case.
No conflicts of interest for any authors.
No external source of funding for authors.
- Kim JH, Gutierrez HR, Lee EY et al (2003). Primary leiomyosarcoma of pulmonary artery; a clinical dilemma. Clinical Imaging, 27(3), 206-211.
- Manmadhan A, Malhotra SP, Weinberg KR et al (2017). Intimal spindle cell sarcoma masquerading as adult on set pulmonic stenosis; a case report and review of literature. J Cardiothorac Surg, (12), 93.
- Chen D, Zhu D, Wang D et al (2006). Clinicopathological and immunohistochemical features of pulmonary artery sarcoma a report of three cases and review of literature. Oncology letters, 11(4), 2820-26.













