Article / Review Article
1Department of Community Medicine, Faculty of Medicine, Khon Kaen University.
2Cancer Unit of Faculty of Medicine, Khon Kaen University.
3Faculty of Medicine, Khon Kaen University,
4Private Clinic, Bangkok
Amornrat Ratanasiri,
Department of Community Medicine,
Faculty of Medicine, Khon Kaen University,
Khon Kaen,
Thailand
6 March 2024 ; 26 March 2024
Cancer is a major health problem all over the world. In Thailand, most women face psycho-social and economic problems, self-stigmatization, and sexual relationships from this gynecologic cancer. Coping mechanisms and special care are needed for those patients in northeast Thailand. The objective of this study was to synthesize knowledge about the illness experiences, coping mechanisms, and special care for these patients since 1985. The review covers the studies produced at Khon Kaen University that were reviewed, synthesized, and analyzed. The results presented that those patients have an impact, not only suffering from these three illnesses but also the feeling of stigmatization. Caregivers, family, community participation, health volunteers, and attending physicians should understand, with kind support to help these gynecologic cancer patients to have a better quality of life.
Keywords: Caring for women, gynecologic cancer, northeast, Thailand
Cancer is a major health problem all over the world (WHO, 2017). Most Thai women face gynecologic cancer illness symptoms, psycho-social and economic problems, sexual relations, self-image, and also stigmatization from this cancer. A coping mechanism was needed for these patients in the northeast of Thailand (Ratanasiri, et al, 1995; Ratanasiri, et al, 2000) (Mongsawaeng, et al, 2016; WHO, 2017).
Gynecologic cancer includes cervical cancer, breast cancer, and ovarian cancer. Cervical cancer is the most common cancer in Thai women (Saenreang, et al, 2019). Breast cancer is the most common cancer in females worldwide. Globally reported that breast cancer accounts for 23% of all cancer in women (Ferlay, et al, 2010). Ovarian cancer is the 6th most common cancer in women in developed Western countries (Silverberg & Liberal, 1987).
In Khon Kaen province, A-population-based cancer registry was established in 1985 (Pengsaa, et al, 1989). This registry covers the population of 1.5 million in 20 districts (Pengsaa, et al, 1990; Pengsaa, et al, 1997). From 1985 to 1989 female population was 700,000 to 800,000. From 1992 to 1994 the incidence rate of cervical cancer in Khon Kaen province and Chiang Mai province was 18.0 and 25.5 per 100,000 female population respectively (Deerasemee, et al, 1999). In Khon Kaen province, it was 16.2 per 100,000 female population during1995-1999 (Sriamporn, et al, 2004). All cervical cancer cases diagnosed from January 1985 to December 1989 in all hospitals in Khon Kaen province were caused by Human Papillomavirus (HPV) (Pangsaa, et al, 1990). That was collected according to the technic described by Maclennan (Maclennan, et al, 1978). Screening by a pap smear for early detection is accepted to reduce the incidence of cervical cancer in Thailand. Well organized system in any primary health care unit by completing family files, including women at high risk of the age 35 and above, and home visits from health personnel help women have a pap smear at least once to give nearly 100 % coverage on each community (Saenrueng, et al, 2019). Nowadays, most Thai girls accept the HPV vaccine from the age of 11 to 20 years old to prevent cervical cancer. Breast cancer is an unknown cause, found only in the abnormality of cells in the breast, milk tube, or mammary glands. Early detection by Self-Examination (BSE) regularly. Breast cancer was not associated with hormonal contraceptives used; when tested with a small number of cases in Thailand (Poosari, et al, 2014). The Age-Standardized Incidence Rate (ASR) of breast cancer in Thailand is highest in Bangkok (34.1), and lowest in Nakhon Phanom province (13.1) (Khunhaprema, et al, 2010). New cases of breast cancer all over the world in 2007 were identified as 1.38 million cases. In recent decades breast cancer incidence has increased rapidly in many developing countries (WHO, 2008). World Health Organization (WHO) reported that ovarian cancer is very commonly found after breast cancer. It is the first-place cause of death in women over the world. Ovarian cancer is an unknown cause. It is associated with heredity, obesity, early menstruation (age less than 12 years old), late menopause (more than 55 years old), infertility, or the use of ovulation stimulation drugs.
Under the method of population-based cancer registry, every case of ovarian cancer diagnosed from every health service center in Khon Kaen province from January 1, 1985 to December 31, 1987 was collected by the cancer unit, Faculty of Medicine, Khon Kaen University, both in passive and active methods. After careful check by the unit’s staff and computerized system, the cases were recorded in the computer for further study. In Khon Kaen province, reported ovarian cancer of 136 cases during 1985-1989. The crude incidence rate varied from 2.72 to 4.89 per 100,000 female population per year, and the age-specific incidence rates varied from 3.88 to 7.01 per 100,000 female population per year (Pengsaa, et al, 1990). The death cases of this ovarian cancer in the same period of time total 20 with the crude mortality rates varying from 0.64 to 1.30 per 100,000 female population per year, while the age-standardized mortality rates varied from 0.81 to 1.94 per 100,000 female population per year (Titapan, et al, 1989). The outcome of ovarian cancer cases after follow-up primary treatment found that most of them fear of death from this illness (Ratanasiri, et al, 1995). Most gynecologic cancer cases suffer from these three types of cancer illnesses that affect to their body and mind.
The study reviewed covers seven studies produced at Khon Kaen University that were analyzed in three steps as follows:
- Synthesized content from staff and students at Khon Kaen University about gynecologic cancer patients in the northeast of Thailand.
- Report illness experiences of three kinds of gynecologic cancer cases.
- Summarized caring procedure for women who face Cervical Cancer, Breast Cancer, and Ovarian Cancer in northeastern, Thailand.
There are three steps to this research result as follows
Step 1: We reviewed illness experiences, coping mechanisms with stigmatizations, and health care system utilization for gynecologic cancer patients in northeastern, Thailand.
We found that illness experiences, and coping mechanisms of 208 cervical cancer patients who received treatment from Srinagarind Hospital from 1998 to 1999, presented that most of them sought treatment from other health care services systems before receiving treatment in Srinagarind Hospital.
Seventy-nine from 208 cases were in-depth interviewed and identified stigmatization by family and community members. Most of them have problems with sexuality. This problem was coped with support from her husband, or/ and the family member.
The follow-up of these cancer patients from the academic staff of the Cancer Unit at the Faculty of Medicine, Khon Kaen University helped people in the community, including the cancer patients, understand this illness, and reduce the patients’ stigmatization (Ratanasiri, et al, 2000).
In the follow-up study of 131 ovarian cancer patients who have primary treatment in Srinagarind Hospital during1985 to 1989, using interviewed questionnaires, and routine letters for follow-up the patients at home at 3,6, and 9-month periods, after primary treatment, with inquiries about their state of health from the Cancer Unit of Faculty of Medicine, Khon Kaen University.
Home visits were arranged after one year for patients who had not responded to the follow-up letter, and were assumed to be still alive.
The results presented that 65% of stage 2 ovarian cancer patients can survive longer than 3-5 years, while the others died.
From our in-depth interviews the ovarian cancer patients at their homes, most of them fear death. (Ratanasiri, et al, 1995).
We followed up 30 cases of breast cancer patients at their homes, during 1999. We found that most of them fear self-image, or/ and divorce from their husbands.
Most of them believed in Karma. Some of them thought that caused by using contraceptive drugs to delay having a baby.
The study about hormonal contraceptive use and breast cancer in 11,414 Thai women with 30 to 69 years who were recruited as participants in the cohort study during the period from 1990 to 2001. The results showed that there was no association between hormonal contraceptive use and breast cancer (Poosari, et al,2014).
Step 2: We reported the caring system for Cervical Cancer, Breast Cancer, and Ovarian Cancer cases as follows:
One case of 45-year-old who works in one province in the northeast of Thailand, but her husband works in a big city in the central part of Thailand. Her husband visits her every month or two months. She has cervical cancer stage 2, but she did not tell her husband about this illness, because she was afraid of staying alone. She suffers from bleeding and pain after sexual intercourse with her husband. In her village belief that women who face cervical cancer caused by multiple partners of married couples made her face stigmatization.
This case presented suffering with cervical cancer symptoms, and fear of divorce from her husband, including fear of stigmatization from the family members, and the community.
The academic staff of the Cancer Unit of the Faculty of Medicine, Khon Kaen University provided essential knowledge of cervical cancer’s symptoms, treatment, and treatment outcome, including prevention of cervical cancer for the patients’ better quality of life. When the villagers understood this illness, they could be reduced stress, and stigmatization.
One case of 34-year-olds who have one daughter of 8 months, and divorced husband. After that, she was diagnosed with Breast Cancer. She always has mood swings and frequent physical abuse of her daughter. The villagers believed that it was because of karma. She had to have her breast removed. and felt the loss of her images. She had to face the stigma and needed special care.
This breast cancer case moved from her house to another village because she did not want to stay in her village. She feared divorce from her husband, and she felt of shyness. Some villagers did not like her because her always moody with her baby made her feel lonely. After the academic staff of the Cancer Unit of the Faculty of Medicine gave mental support to her, she felt better and came back to her village. Her husband understood and lived with her and their baby.
One case of 56 years old who is single. She was diagnosed with Ovarian Cancer stage 4 with an unknown cause. She passes away after treatment for two years.
This case died after the diagnosis only two years ago made other ovarian cancer cases in the same community fear death, and believe that ovarian cancer cannot be cured. The academic staff of The Cancer Unit need to provide a prevention program for this illness to the villagers. After the villagers understood this disease, they felt better and avoided of risk factors of this ovarian cancer.
Step 3: From Figure 1 we summarized coping mechanisms and caring for three kinds of gynecological cancer as follows:
Cervical Cancer caused by Human Papillomavirus (HPV) (WHO, 1986). In 2022, the statistics in Thailand reported that Cervical Cancer is 3rd place in the top 5 Cancer among Thai people. It reported 140,000 new cases or 400 cases per day. Approximately 4,500 cases die per day (National Cancer Institute of Thailand, 1994), or an average of 8-10 cases die per day. Preventing this disease is to vaccinate the HPV vaccine for Thai girls aged 11 years old to 20 years old, including avoiding having multiple sexual partners. To control this illness is reducing risk factors of cervical cancer, and screening by Pap smear, HPV DNA Test, Colposcopy examination, or endocervical curettage. This illness can be treated by Surgery, Radiation, Chemotherapy, or Combined treatment. Most patients suffer from this illness, face stigmatization, fear of divorce from husbands, and suffering from having a sexual relationship. Caregivers and attending physicians should be understanding and help to improve those patients’ quality of life.
Breast Cancer is the first cancer found in Thai females. It is unknown cause, found only abnormality of cells in the breast. The statistics report in Thailand in 2022 that 80% found an abnormality in the milk tube, and 10% found an abnormality in mammary glands. To prevent this illness Breast Self-Examination (BSE) on a regular basis. To control this disease, pay attention to the twelve risk factors of breast cancer, including sex, ethnicity, having a child, sex hormones, age, obesity, breast tightness, history of drug use for breast treatment, heredity, alcohol drinking, cigarette smoking, and had breast cancer before screening by Clinical Breast Examination (CBE), or Mammogram, or Ultrasound, or Needle biopsy.
Ovarian Cancer is an unknown cause. It is associated with heredity, or obesity, or early menstruation (age less than 12 years old, or late menopause, or age more than 55 years old), or infertility, or the use of ovulation stimulation drugs. World Health Organization (WHO) reported in 2014 that ovarian cancer is very commonly found after breast cancer. It is the first-place cause of death in women all over the world. Prevention of ovarian cancer can be done by eating a balanced diet, exercising regularly, having emotional stability, and receiving treatment for ovulation disorder. Control by reducing risk factors e.g. avoiding eating fatty food, living in a good environment, and far from chemical substances. Screening for ovarian cancer. In case of having a risk factors should see an obstetrician regularly, have an internal inspection annually, or do blood tests to find more protein CA-125 than normal. Treatment is different in the 4-stages of cancer. In stage 1, cancer is in the ovary. Stage 2 to 4, cancer has spread to other organs. Treatment includes surgery, chemotherapy, radiotherapy, and combined treatment. (Figure1).
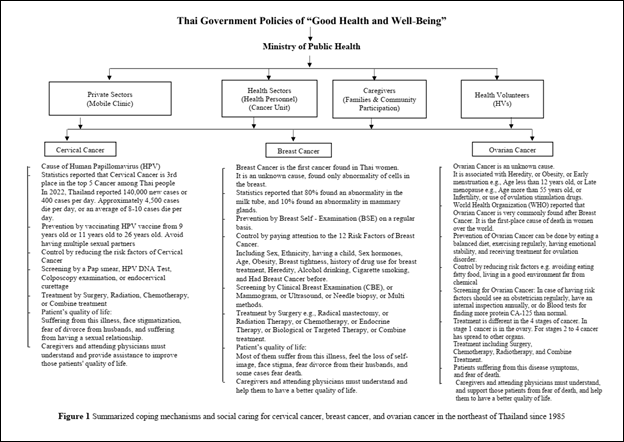 Figure 1: Summarized coping mechanism and social caring for cervical cancer, and ovarian cancer in the northeast of Thailand since 1985
Figure 1: Summarized coping mechanism and social caring for cervical cancer, and ovarian cancer in the northeast of Thailand since 1985
Our reviewed research found that most cervical cancer, breast cancer, and ovarian cancer showed suffering from illnesses symptoms to the body and mind. Most of them face stigmatization because people around them believe in karma, and think that cancer cases do something not good, making them get cancer. Most gynecologic cancer cases felt fear of death, fear of family relations, and community member relationships. Some cervical cancer cases felt pain or had bleeding per the vagina from having sexual relations with their husband, but she did not tell them because she fear divorce from her husband. Breast cancer cases felt fear of death, fear of her self-image after breast surgery, and also fear of divorce from her husband. Ovarian cancer was suffering from this disease symptoms, and fear of death. Similar to the study of Srimoragot which presented that cancer cases also cause psychological damage during treatment. It induced severe stress, loss of self-esteem, and felt low morale (Srimoragot, et al, 1994). Same as previous studies, cervical cancer is the most significant disease affecting women’s health in Thailand (Chutidumrongpan, et al, 1996; Chugiart, et al, 1996; Ratanasiri, et al, 2000). Some breast cancer cases were anxious about eating food and medicine e.g. fatty food, or contraceptive drugs, or hormone use for menopausal symptoms (Ewertz, et al, 2005). Similar to Silverberg’s study that presented 5% of ovarian cancer deaths from this cancer in the United States (Silverberg & Lubera, 1987). Previous studies in the northeast of Thailand presented that ovarian cancer showed rather low incidence when compared with other countries in the world. It was not the major cause of death in the Khon Kaen female population (Titapant, et al, 1989). From our follow-up study of these ovarian cancer cases, most of them still feel fear of death (Ratanasiri, et al, 1995). Most of them face stigmatization because people around them believe in karma. thought that cancer cases did something not good before they got cancer. The caregivers and attending physicians should understand these three types of gynecologic cancer give mental support to them and help them to have a better quality of life.
Health personnel in the health sectors, and private sectors, including caregivers, family, community participation, and health volunteers (HVs) must understand these three illnesses and kindly support those patients. In conclusion of our reviewed research, we found that most gynecologic cancer cases face these illness symptoms and affect their mind and body in many aspects.
The caregivers and attending physicians should understand those patients, treat them, mentally support them, and help them to have a better quality of life.
Other health personnel in the health sectors, private sectors, including family members, community participation, and health volunteers (HVs) good reactions, and home visits from the academic staff of Khon Kaen University made these three types of cancer in women, more understanding of their illness symptoms and made them better coping with these problems.
We thank all the respondents for their valuable contribution to our studies. The cancer unit of the Faculty of Medicine for data support. The Faculty of Medicine at Khon Kaen University for funding support.
The research reviewed was approved by the Ethics Committee for Human Research of Khon Kaen University. Most research studies were based on secondary data. Some of them gave more information during in-depth interviews. Those who volunteered signed the consent form.
- WHO. (2017). International Classification of Diseases for Oncology, 3rd Ed (ICD-0-3) (Internet), Word Health Organization. Retrieved from: https://www.who.int/standards/classifications/other-classifications/international-classification-of-diseases-for-oncology
- Mongsawaeng, C., Kokorn, N., Kujapan, J., Norkaew, J., Kootanavanichpong, N., Chavenkun, W., Ponphimai, S., Kaewpitoon, S. J., Tongtawee, T., Padchasuwan, N., Pengsaa, P., Kompor, P., & Kaewpitoon, N. (2016). Knowledge, Attitude, and Practice Regarding Cervical Cancer among Rural Community Women in Northeast Thailand. Asian Pac J Cancer Prev, 17(1), 85-8. DOI: https://doi.org/10.7314/apjcp.2016.17.1.85
- Ratanasiri, A., Hedley, A. J., Pengsaa, P., & Vatanasapt, V. (1995). The Outcome of Follow-up study and primary Treatment of Ovarian Cancer at Srinagarind Hospital during 1986 to 1989. Thai Cancer Journal, 21(3-4), 96-107.
- Ratanasiri, A., Boonmongkon, P., Upayokin, P., Pengsaa, P., & Vatanasapt, V. (2000). Illness experience and coping with gynecological cancer among northeast Thai female patients. Southeast Asian J Trop Med Public Health, 31(3), 547-53. Retrieved from: https://pubmed.ncbi.nlm.nih.gov/11289018/
- Saenrueang, T., Promthet, S., Kamsa-Ard, S., & Pengsaa, P. (2019). Cervical Cancer in Khon Kaen, Thailand: Analysis of 1990-2014 Incidence Data and Prediction of Future Trends. Asian Pac J Cancer Prev, 20(2), 369-75. DOI: https://doi.org/10.31557%2FAPJCP.2019.20.2.369
- Ferlay, J., Shin, H.R., Bray, F., Forman, D., Mathers, C., & Parkin, D.M. (2010). Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer, 127(12), 2893-917. DOI: https://doi.org/10.1002/ijc.25516
- Silverberg, E., & Lubera, J. (1987). Cancer statistics, 1987. CA Cancer J Clin, 37(1), 2-19. DOI: https://doi.org/10.3322/canjclin.37.1.2
- Pengsaa, P., Vatanasapt, V., Titapant, V., Udomthavornsuk, B., & Sri-Amporn, S. (1989). The impact of mass screening to cervical cancer in Khon Kaen province. Thai cancer J, 15, 11-17.
- Pangsaa, P., Udomthavornsuk, B., Titapan, V., & Vatanasapt, V. (1990). The Epidemiology of Ovarian Cancer in Khon Kaen 1985-1989. Epidemiology of Ovarian Cancer, 2(2), 95- 101. DOI: https://doi.org/10.21037/cco-20-34
- Pengsaa, P., Vatanasapt, V., Sriamporn, S., Sanchaisuriya, P., Schelp, F. P., Noda, S., Kato, S., Kongdee, W., Kanchanawirojkul, N., & Aranyasen, O. (1997). A self-administered device for cervical cancer screening in northeast Thailand. Acta Cytol, 41(3), 749-54. DOI: https://doi.org/10.1159/000332698
- Deerasamee, S., Matin, N., Sontipong, S., Sriamporn, S., Sriplung, H., Srivatanakul, P., Vatanasapt, V., Parkin D M., & Ferlay, J. (1999). Cancer in Thailand volume II,1992-1994. IARC Technical report no. 34. Bangkok, Thailand. Medical Publisher.
- Sriamporn, S., Parkin, D. M., Pisani, P., Suwanrungruang, K., & Pengsaa, P. (2004). Behavioral risk factors for cervical cancer from a prospective study in Khon Kaen, Northeast Thailand. Cancer Detect Prev, 28(5), 334-9. DOI: https://doi.org/10.1016/j.cdp.2004.01.005
- World Health Organization (2014). Comprehensive cervical cancer control: A guide to essential practice. 2nd ed, WHO Press. Retrieved from: https://www.who.int/publications/i/item/9789241548953
- World Health Organization. (1986). Control of cancer of the cervix uteri. Bull WHO, 6(4), 607-18. Retrieved from: https://pubmed.ncbi.nlm.nih.gov/3490930/
- National Cancer Institute of Thailand. (1994). Statistics Report of Gynecological Cancer (1994);23.
- Maclennan, R., Muir, C., Steinitz, R., & Winkler, A. (1978). Cancer registration and its techniques. IARC Sci Publ 1971(21), 1-234. Retrieved from: https://pubmed.ncbi.nlm.nih.gov/378815/
- Poosari, A., Promthet, S., Komsa-ard, S., Suwanrungraung, K., Longkul, J., & Wiangnon, S. (2014). Hormonal contraceptive use and breast cancer in Thai women. J Epidemiol, 24(3), 216-20. DOI: https://doi.org/10.2188%2Fjea.JE20130121
- Khuhaprema, T., Srivatanakul, P., Attasara, P., Sriplung, H., Wiangnon, S., & Sumitsawan, Y. Eds. (2010). Cancer in Thailand 2001-2003. Bangkok: Bangkok Medical Publisher. Retrieved from: https://ghdx.healthdata.org/record/thailand-cancer-thailand-volume-v-2001-2003
- World Health Organization. International Agency for Research on Cancer. (2008). World Cancer Report 2008. Boyle, P., & Levin, B. (Eds). The International Agency for Research on Cancer, Lyon, France. Retrieved from: https://publications.iarc.fr/Non-Series-Publications/World-Cancer-Reports/World-Cancer-Report-2008
- Titapant, V., Pengsaa, P., & Vatanasapt, V. (1989). Epidemiology of ovarian cancer in Thailand: Pilot study from Khon Kaen Population–based cancer registry +. Srinagarind Medical Journal, 4(3), 175-82. Retrieved from: https://li01.tci-thaijo.org/index.php/SRIMEDJ/article/view/13499
- Srimoragot, P. (1994). The effects of supportive counseling on perceived illness in self-esteem and morale in cervical cancer patients undergoing radiotherapy in 1994. Mahidol University. Bangkok. (In Thai)
- Ratanasiri, A., Boonmongkon, P., Upayokin, P., Pengsaa, P., & Vatanasapt, V (2000). Chutidumrongphan, A. An application of the health belief model and group process to promote PAP smear attendance behavior among women in Promkiri district of Nakorn Sri Thammaraj Province. Mahidol University Graduate Studies: MSc. Thesis (Public Health), 1996. Cite in Illness Experience and Coping with Gynecological Cancer among Northeast Thai Female Patients. Southeast Asian J Trop Med Public Health, 31(3), 547-553. Retrieved from https://www.tm.mahidol.ac.th/seameo/2000_31_3/25-2400.pdf
- Chugiart, N. (1996). Ways of Motivating Rural Women in Dunkhuntod District of Nakorn Rachasima Province to attend PAP Smear test.Mahidol University; Graduated Studies: MSc Thesis (Public Health), 1996. Cite in Ratanasiri A, Boonmogkon P, Upayokin P, Pengsaa P, & Vatanasapt V (2000). Illness Experience and Coping with Gynecological Cancer among Northeast Thai Female Patients. Southeast Asian J Trop Med Public Health, 31(3), 547-553 Retrieved from https://www.tm.mahidol.ac.th/seameo/2000_31_3/25-2400.pdf
- Ewertz, M., Mellemkjaer, L., Poulsen, A.H., Friis, S., Sørensen, H.T., Pedersen, L., McLaughlin, J.K., & Olsen, J. H. (2005). Hormone use for menopausal symptoms and risk of breast cancer. A Danish cohort study. Br J Cancer, 92(7), 1293-7. DOI: https://doi.org/10.1038%2Fsj.bjc.6602472













