Article / Case Report
BİRUNİ UNİVERSİTY Istanbul.
Tahir Ataözden
BİRUNİ UNİVERSİTY
Istanbul.
13 November 2023; 9 December 2023
A 14-month-old baby boy was admitted to the Dental Treatment Center of the Faculty of Dentistry of Kafkas University in May 2022 with a green tree fracture in the left mandibular condyle. According to the information given by the family of our patient, she fell from the sofa and became unable to breastfeed due to the effect of trauma. After the clinical and radiological examination of our patient, a left mandibular green branch fracture was detected. Panoramic x-rays could not be taken due to the fact that it was a baby, only computed tomography was performed, and since our patient was a 14-month-old baby, conservative treatment without maxillomandibular fixation was thought to be appropriate, followed by mechano- physiotherapy.
Keywords: Condyll, Green Branch, Mechano, Treapy.
Mandibular Condyle Prosses fractures are common, with between 29% and 40% of facial fractures belonging to Condyle Prosses fractures. In addition, between 20% and 62% of all Mandible fractures belong to Condyle Prosses fractures, these are very high rates, Maxilla Mandibular fractures in children are less common than in adults, and the fracture rate increases with age. Serious differences are observed between adult fractures and pediatric fractures due to incomplete bone development. The pathology of pediatric bone fractures is very different from the pathology of normal adult fractures. We can see this type of fracture in children mostly in falling, bicycle and other toy accidents. Although the treatment of condylar fractures in infants and children is controversial; There are 2 types: 1-Open reduction, 2-Closed reduction, \ non-surgical conservative approach, mechanotherapy. Generally, non- displaced green branch fractures are seen in infants and children. In this type of fracture, non-surgical closed reduction treatment is preferred. If age and dentition are appropriate, maxillary fixation or maxilla mandibular fixation is applied. In addition, the patient is followed up with physiotherapy and mechanotherapy. We followed our patient for 6 months in our clinic, and we believe that this mechanotherapeutic event accelerated the recovery due to the necessity of sucking his mother. Achieving normal occlusion is the 1st priority. In patients with \milk teeth\ that have completed or have completed this dentition, normal occlusion can be achieved even if there is a slight shift in the midline with relatively bimaxillary fixation, but in cases where it cannot be achieved, there is no other method other than mechanotherapy.
Our 14-month-old baby boy was admitted to Kafkas University Faculty of Dentistry Dental Treatment Center in March 2022 with left mandibular condyle fracture trauma. According to information from his mother, he fell on his cheek from the plastic slide. Since the environment is plastic, there are no incisions and injury marks. Since it was a baby, the panoramic could not be obtained, and the result was that our patient was put to sleep and computed tomography was taken. Necessary medical drugs were prescribed to prevent edema. Our patient’s mouth opening was close to normal with 22-25 mm, but since the upper central and lateral occlusions can continue the lower central and lateral parts of the lower jaw, a shift of 2-3 mm was detected in the recording. For the first 3-4 days, our baby could not suck his mother due to pain and suffering and was fed with soft foods. After the 4th day, she started to suck the mother again and the mechanotherapeutic effect began to show itself. As a result of the conservative treatment approach we planned and the planning made with the family, it was recommended that our baby do mouth opening and closing exercises at certain times of the day. Our patient was called every 20 days and observational and physical examination was performed. It was observed that the mouth opening was 30 mm, which was normal limits. It was observed that the shift in the midline gradually decreased, and family impressions were that there was no abnormality in the baby. A signed consent form was obtained from the patient’s parents in accordance with the Declaration of Helsinki.
Condylar Fractures are treated in children and infants with non-surgical methods and detailed follow-ups as a result of long periods. Unfortunately, when children younger than 6 years of age have an excessively displaced condyle fracture, open reduction has always been the first choice, even considering the risk of nerve damage from the surgical method. However, if there is no displacement, the treatment is continued with closed reduction. This is because surgical access to the Tempora Mandibular Joint area is difficult and risky, and repositioning of regional segments is quite difficult. The most important factors in deciding on open or closed reduction are the status of the existing occlusion and the age of the patient. Generally, the age of the patient is less than 6 years and the distalization in the occlusion is absent or does not exceed 1-2 mm. When we took these criteria as a repercussion, as we saw in many researchers who were the source of our research, a strict follow-up, mechanotherapy and natural attraction of the chewing muscles (especially the mechanotherapeutic breast milk sucking movement that occurred in our 14-month-old baby) and an excellent recovery was achieved with closed reduction in a minimum of 2 to a maximum of 6 months. In their 2012 study, Su- Seong Park and Keun-Cheol Lee examined the disagreements on this issue in order to be able to criticize the treatment methods for condylar fractures in the most perfect way, and stated the misunderstandings about today’s treatment strategies one by one in this study. Mandible condyle fracture is so common that almost 30-40% of all mandible fractures are condyle fractures only. In addition, approximately 40% of pediatric injured patients have mandibular condyle fractures (Su Seong & Keun Cheol, 2012). The mandibular condyle is a region that plays a key role in the opening and closing of the mouth, and since it causes functional and aesthetic problems such as facial asymmetry, it is very important to perform a correct reduction. In open reduction techniques, which are mandatory in some cases, it has been observed that using 2 mini-plates instead of using a single mini-plate provides better stability (Ellis, 1986). Since Maclennan (Akbulut et al., 2013) advocated closed reduction for 180 patients with mandibular condyle fractures in 1952, complications in mandibular condyle fractures have been observed to be significantly reduced, and closed reduction has been generally accepted for about 10 years. However, Blevins and Gores (Mac Lennan, 1952). observed that after conservative treatment in 140 patients, only 13% of them had a good prognosis, and 50% of the patients had a narrowing of the mouth opening up to 28 mm. In addition, various bite and pain problems were found in 36% of the patients. In their study, Silvennoinen et al. (Blevins, 1965). found restrictions in opening the mouth in 15% of 92 patients, and malocclusion and permanent mandibular deviation in 17% of the patients. Eliis et al. (Silveron, 1979). stated that complications such as scarring of the facial nerve or partial paralysis were seen in open reduction, while complications such as chronic pain, mal occlusion, facial asymmetry, and limitation of movement were encountered in closed reduction. As a result, it is determined that extraordinary developments in surgical techniques in recent years have turned the needle towards open reductions. However, as in our 14- month-old infant patient and in all pediatric patients younger than 6 years of age, closed reduction and strict follow-up are considered more appropriate in conservative and mechano-therapeutic and green branch fractures, that is, bending fractures, which have the possibility of improvement with muscle function.






Rear shooting Aftermath of trauma

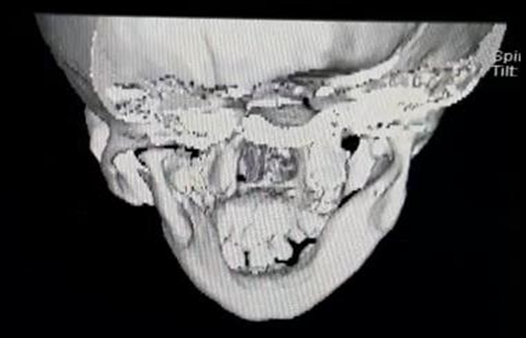
Front shot Aftermath of trauma Rear shooting
What it looks like after recovery

Bottom shot
What it looks like after recovery
- Su Seong, P., & Keun Cheol, L. (2012). Criticism of treatment modalities in condyle fractures. 62, 155-163.
- Akbulut, N., Tümer, M. K., & Ertem, S. Y. (2013). 10, 26-71.
- Mac Lennan. (1952). Complication ratios in closed reductions. 29, 232-237.
- Blevins. (1965).Gores Prognosis rates of closed reductions. 67, 25-30.
- Silveron. (1979) Complications of Arc Closed reduction. 26, 32-35.
- Ellis. (1986) Complications of open and closed reductions of arc. 67, 25-30.