Article / Research Article
1Department of Nutrition, Tel Hai Academic College and Private Eating Disorder Centre, Israel
Moria Golan
Department of Nutrition
Tel Hai Academic College and Private Eating Disorder
Centre
Israel
6 January 2021 ; 21 January 2021
Clarifying terminology in psychological science is crucial to develop suitable practices and improve treatment effectiveness.
To provide theoretical framework which integrates the scientific literature regarding the transdiagnostic dimensions in the eating disorders (ED) spectrum: self-agency, mentalization, self-control and self-regulation. In addition to introducing a newly developed eating and control style axis, (ECOSA), it focuses on better conceptualizing the complex interaction between eating style, control conditions, and the impact of the “emotional brain” versus the “thinking brain.”
Electronic searches of MEDLINE, EMBASE, and PsycINFO, were performed on April–May 2020 using the keywords Self agency or mentalization or reflective functioning or self-regulation or emotion regulation or self-control or self-agency and eating disorders.
There are numerous scientific literatures related to eating disorders. However, only two were related to all the dimensions discussed in this manuscript. Most reviews have focused on a single diagnostic category or two dimensions. Only, one study reported the results of mentalization-based treatment (MBT). ECOSA provides an example of a tool that may be used to promote self-agency in the management of eating disorders.
To enhance perception of ownership over an effector (self-agency), clinicians need an instrument that assists in exploring the agent’s inner intentions. ECOSA may be used by all those who seek further clarity regarding the association between pathological eating behaviors, self-regulation and under- or over-c
Keywords: Eating Disorders, Mentalization, Self-regulation, Self-control, Self-agency
To address the crucial need to improve the profound suffering and impact of eating disorders on a person’s life, therapeutic strategies aim to target various dimensions in eating disorders, thereby curing, and helping patients [1]. Impaired emotion regulation (ER) and self-control as well as mentalization and self-agency are reported as transdiagnostic dimensions considered in a variety of psychological disorders, including eating disorders (EDs) and disordered eating symptoms [2,3,4].
Self-control is what people use to restrain their desires and impulses. More precisely, it can be understood as the capacity to override a response (and substitute another). It is a part of self-regulation [5]. Most self-regulation occurs in one of four following spheres:
- regulation of distracting thought;
- regulation of mood and emotions;
- resistance to tempting desires, impulses and compulsions;
- Regulation of execution, performance or functioning.
Exerting self-control, is an effortful process. If it is over-consumed, people may be in a temporarily depleted state and then may fail to exert self-control or adaptive coping or functioning [6]. This is occasionally the case for those who excessively control their body and/or eating, and those who struggle to maintain their weight [7]. Thereafter, they may experience passionate or increased desires to eat, resulting in overeating and sometimes purging behaviors.
People with various grades of being underweight – anorexia nervosa (AN) and or Avoidance restrictive feeding intake disorder (ARFID)- AN and ARFID) often present obsessive-compulsive manners of over-controlling their eating and body shape as a mechanism to regulate their anxiety from maturity fears, emotional and development growth, interpersonal distrust, direct communication, traumatic history and as a strategy of harm avoidance due to personal characteristics such as perfectionism [8].
People with obesity, overweight or suppressed weight often report on under-controlled behavior style being expressed in impulsivity, over eating although the wish to restrict eating, emotional eating and even binging [7]. Their eating behaviors serve as a mechanism to self-regulate their controlling emotions (intolerance to negative emotions), depression, and sometimes vulnerability to obesity and oversensitivity to appearance.
Extensive support exists in the eating disorder’s literature connecting eating pathologies and mentalization [9]. Mentalization or reflective functioning, is defined as “the mental process by which an individual implicitly and explicitly interprets the actions of himself and others as meaningful on the basis of intentional mental states” [10]. The ability to understand and express experiences of the self and others, assists the individual to cope with various stressors, to regulate internal and external affects, and to practice good interpersonal relationships [11].
Enhancing mentalization regarding the connection between intolerance to negative emotions, anticipation anxiety, negative urgency and eating pathologies was found to be effective in improving self-agency (the sense that some problems/behaviors are self-generated), and thus, improvement in eating behaviors and enhanced well-being [12]. Mentalization-based Treatment (MBT), which is grounded in John Bowlby’s Attachment Theory and Ecological Systems Theory, is widely presented in the scientific literature of eating disorders. Yet, most works describe the general process linking negative emotions and distress intolerance with various eating behaviors, without clarifying the association with the individual’s control style and the individual’s agency regarding the battle between the “emotional” and “frontal-cognitive” brain in the various categories of eating disorders. Moreover, most reviews have focused on a single diagnostic category or two dimensions while here we describe all the above-mentioned dimensions, through the whole eating disorders spectrum. Eating and Control Style Axis (ECOSA), provides an example of a tool that may be used to promote self-agency in the management of eating disorders.
The aim of this manuscript is to provide theoretical framework which integrates the scientific literature regarding the dimensions of self-agency, mentalization, self-control and self-regulation and the eating disorders (ED) spectrum as well as propose an example of a newly integrative conceptualized tool—Eating and Control Styles Axis (ECOSA)—to improve the mentalization and self-agency of people with eating disorder.
Emotion is a “component of affect, a broader concept that includes stress, mood, and impulses” [13]. Emotional Regulation (ER) refers to the ability to manage and cope with discomfort with a variety of negative emotions, (i.e. fear, disgust, anger, sadness, shame) or the perceived absence of something necessary/desired, e.g., emptiness), as well as positive emotions such as strong positive excitement. In this process, actions are directed to contain and regulate current emotions, as well as to control the associated response, intrinsically (within self), and extrinsically (towards others) [14].
ER has an action-tendency designed to resolve the stress or the over-excitement, rather than to dwell on the affect and unmoderated response that might accompany those situations and avoid a maladaptive pattern of responses. The different responses may differ by response-focused regulation or antecedent-focused regulation, which occurs early in the emotional sequences [15].
Oversensitivity to threatening cues and difficulties in regulating negative emotional states and impulses during the lifespan have also been recognized as a transdiagnostic risk/maintenance factors for general psychopathology as well as eating disorders [16,17,18]. Both may lead to maladaptive or dysfunctional reactions by increasing the awareness to the relevant cue and often by employing either over-controlling or under-controlled behaviors as avoidance defense mechanism [18,19].
Exerting control over-eating by restrictive eating and controlling weight, enables individuals to avoid the negative affect associated with various difficulties. This is due to the sense of self-control “because it is perceived as successful behavior in the context of perceived failure, in all other areas of functioning” [20,21].
Excessive control on eating may also serve as an avoidance defense mechanism through distracting individuals from their negative emotions by remaining preoccupied with weight and food (“my main problem is my weight, as long as I don’t lose weight I avoid eating with friends”) as well as through projection and displacement of feelings of confidence and security on food and body (“when I feel controlling and confidence in my body, I experience it as if I am self-regulated and I am confident”). Moreover, the experience of control obtained via controlling eating and the body is displaced toward the whole-self. Instead of dealing with negative emotions elicited by uncontrolled and stressful situations and behaviors, people with Emotional Disorders (EDs) often unconsciously achieve relief through exerting control over food and weight or by eating as much as they want (the illusion of freedom) or alternatively exactly the way they want (“only my way”) and later compensating with purging behaviors.
The intolerance to negative emotions may be unconscious; still, when people are aware of this, they still do not adapt a positive coping behavior due to various deficits, such as a lack of understanding these emotions; inability in emotion differentiation, inability to employ flexibly, lack of regulation skills and strategies— often observed among individuals with anorexia nervosa [22,23].
Negative urgency, similar to distress intolerance, is also considered as a transdiagnostic risk/maintenance factor for psychopathology. Urgency refers to the notion that you must have the object/the relief immediately and often it produces an uncontrolled urge [18]. Engaging in harmful behaviors to avoid negative internal experiences because of an intolerance of negative urgency is a well-established predictor of the onset and maintenance of a range of compulsive behaviors and syndromes such as EDs and substance abuse. It holds back the ability to engage in adaptive and valuable activities and contributes to functional impairment [2,22]. People with eating disorders tend to respond to immediate negative emotions by a negative reward such as overeating or fasting as opposed to pursuing alternative positive reinforcers. Distress intolerance and high impulsivity were common predictors of bulimic symptoms among people with eating disorders, when experiencing a negative affect [18,24]. Elevated negative affect and higher degrees of negative urgency in women with EDs positively predicted impulsive response and purging frequency [25].
Impulsivity, a tendency to act prematurely and without foresight and preference for smaller but immediate gratification, over larger and delayed rewards—also called heightened delay discounting—varies across psychiatric disorders. Binge eating and purging behaviors are often considered to be predicted by impulsivity with stronger predictive effects than lack of persistence, lack of planning, sensation seeking and positive urgency.
Impulsivity may manifest due to attention impairment or low conscientiousness, sensation-seeking, impaired executive functioning activity and failure to take the right decisions, as well as, urgency to consume something to achieve a sense of relief from hunger or negative emotions [26]. Langer et al. reported that among different categories of EDs, there is hierarchy of occurrence of impulsivity features [27]. “Cognitive impulsivity, motor impulsivity, and global impulsivity were the most prominent in the Anorexia Nervosa (AN) binging/ purging type, while the lowest score in those constructs were observed among patients with restrictive AN. Those with binging/purging AN demonstrated a greater difficulty delaying gratification compared with people with other categories of EDs who demonstrated a preference for a higher, delayed reward.”
The different types of ER patterns as well the different control styles have different neural patterns. Behavioral regulation (response) was suggested to be supported by the subcallosal cingulate cortex (SCC) and the dorsal pathway, and the cerebellum and/or prefrontal regions operating on subcortical and brainstem structures. While antecedent-focused regulation (avoidance) was suggested to be supported by circuits involving lateral and medial portions of the orbitofrontal cortex (OFC), the lateral and ventromedial portions of the prefrontal cortex (lPFC &vmPFC), the anterior and posterior cingulate cortices [15]. Trafton and Gifford suggested that the different neurobiological substrates, underlying and modulating reward learning and response, may mediate emotions ranging from tolerance to distress [28].
People with restrictive anorexia nervosa often report an increased capacity to delay rewards and tolerate asceticism and restrictions, and thus, may override the drive to eat. On the other hand, people with binge eating disorder (BED) or (BN) often report on a reduced ability to delay gratification [29]. Neuroimaging evidence has suggested that the ability to delay gratification is enhanced when the rewarding value of food is decreased (satiety and calming states), and it decreased following hunger and spared, states in which the rewarding value of food is increased [30]; thus, emotion dysregulation is often associated with excess weight because of lower delayed gratification [29]. A hungry individual that employ extreme restriction usually face difficulties in delaying food gratifications [25].
To manage the pathological symptoms expressed by over-controlled or under-controlled behaviors, caused by distress intolerance, difficulties in self-regulation, impulsivity and in delaying gratification, the individual needs to be self-acknowledged and have a sense of self-agency about these difficulties, as well as possess motivation to employ adaptive healthy defense and coping strategies. Healthy self-control requires the incorporation of mentalization and self-agency processes.
Diminished mentalization is considered as a common mediator between self-regulation and variety of disorders and behavioral problems [10]. Children who demonstrate distress intolerance and whose parents fail to provide accurate and adequate empathy, mentalization, and validation, may experience an escalation of negative emotions and a need to displace them through controlling behaviors or alternatively, demonstrative behaviors [31,32]. People with EDs often display a diminished ability to mentalize experiences, a greater difficulty in differentiating between physical and emotional states and between their own and others’ experiences, and the tendency to attribute causality to oneself and other interpersonal experiences [3,33]. Due to difficulty in understanding and tolerating their own and others’ internal experiences as well as intense or disconnection with their own emotions and body sensations, people with EDs often report problems in constructing a personal positive narrative over time in relation to their feelings, experiences as well as their behaviors [34,35].
Deficiency in imaginative mental activity about intentional mental states and in mentalization, and thus, emotion dysregulation and negative urgency may lead to the use of eating disorders as a concrete means of expressing and relieving feelings and thoughts, as well as regulating drives and emotions [36,37]. All these had been demonstrated as precursors to binge eating [38,39]. The capacity for mentalization is “thought to be a prerequisite for a sense of agency in relation to emotions and behavior” [40].
A sense of agency refers to the sense that some problems/ behaviors are self-generated (Moor, 2016) and thus, the individual should manage it. In terms of symptoms, self-agency reflects how strongly the person perceives his impact on his or her problematic experiences and behaviors [32]. Sense of agency plays a key role in directing action against harmful decisions and behaviors [41]. To achieve it, the agent must first perceive ownership over an effector (which is hard with a lack of mentalization capacity). Second, they must mitigate their personal intentions. Only then they may have the ability to take responsibility and act through the ambivalence, as it often pertains to eating and weight status in eating disorders. An abnormal sense of agency may provide the grounds for diminished responsibility, as often it occurs when someone is required to cope with pathological symptoms. fMRI studies demonstrated that explicit judgment and implicit processing of self-agency are mediated by different brain mechanisms located in ventral premotor cortex, the supplementary motor area, and the cerebellum along with the posterior parietal cortex (PPC), posterior superior temporal sulcus (STS), and the insula [42].
Improving mentalizing and the mentalization process recently has been a topic of focus of many psychotherapy approaches [43]. Psychotherapy may help repair developmental and environmental deficits by recreating the mentalizing effects of the interactional matrix of early childhood by producing a better atmosphere and conditions for growth. This will in turn enable the individual to conscious awareness, ability to understand experiences and facilitate a sense of mental agency [12,44]. Fonagy and Bateman stated that mentalization assists the patients to “become able to think more clearly about the mental processes that underlie their actions” [45]. They further proposed that patients need assistance with understanding the content of their associations, as well as recognizing the existence of the thoughts and feelings that they are experiencing to further develop a sense of agency that may determine future decisions and outcomes [32]. Leventhal’s self-regulatory model shows that following exposure to stimuli, the individual makes sense of the stimuli both cognitively (understanding it) and emotionally (feeling it), which leads to the individual choosing appropriate coping strategies [46]. Nevertheless, a randomized trial of mentalization based therapy for eating disorders (MBT-ED) reported a high drop-out rate, which made the interpretation of the results difficult [47].
So far published manuscripts lack instrumental ideas about how to facilitate mentalization-based therapy for the management of eating disorders. We found that only few encompass all the above-mentioned dimensions to enhance an individual’s self-agency regarding the symptoms of eating disorders.
Impulsivity, difficulties in self-control, and regulating negative emotions are considered as transdiagnostic characteristics of people with EDs. It is essential to provide them with a sense of understanding of their extreme behaviors, reflecting uncontrolled and/or overcontrolled patterns and provide the strategies to empower the “thinking brain” over the “emotional brain”. As Fonagy et al. suggested, clearly thinking about the mental processes that influence people’s actions is a prerequisite for a sense of agency and better choice behavior [32]. As the spectrum of individuals who develop EDs is broad, there is a need to address the gap between theory and practice regarding the mentalization process for people with various pathological eating behaviors.
A comprehensive conceptualization axis (ECOSA) was developed to demonstrate people’s choice of a specific eating style (over- or undereating, restriction, or binging), their control style (underbalanced or overcontrol), and weight status on a continuous axis (Figure 1). As most people would like to perceive themselves as “rational,” they may gain from understanding the role of the “thinking brain” versus the “emotional brain” in respect to these behavioral and control decisions. The top part of the axis presents the eating style and weight status; below is the control axis, and the bottom part presents the associated brain activity.
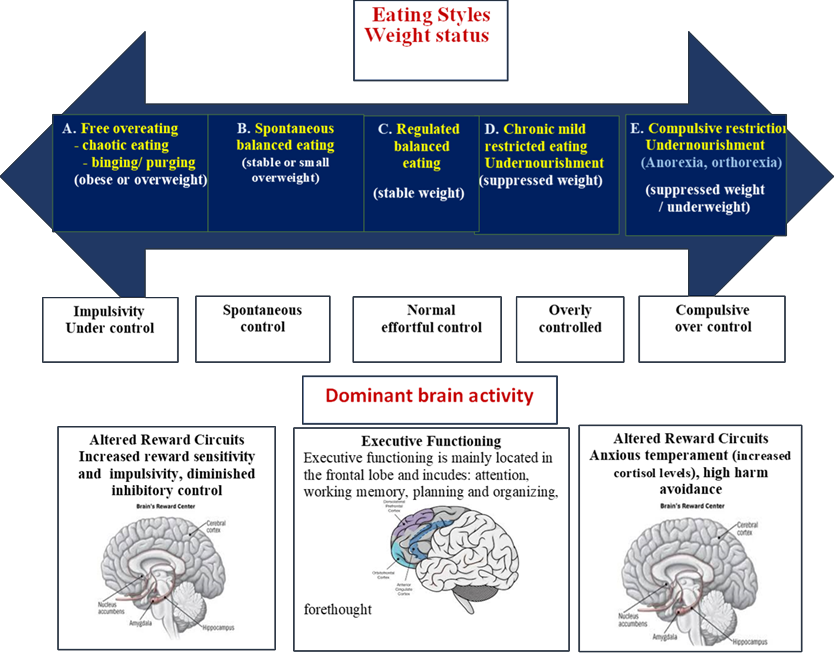
Figure 1: Eating and Control Styles Axis (ECOSA) and the dominant brain activity
On the left end of the continuous axis, the under-controlled eating group is shown (A). Individuals in this group usually behave according to their passions, overeat during mealtime, and frequently consume unscheduled snacking. They tend to have difficulties in delaying gratification and often eat impulsively. Food is considered an aid and a means to distract or cope with stress and negative emotions. In this group, impulsivity reflects decision-making that occurs with limited forethought and diminished inhibitory control. Impulsive tendencies to act rashly, due to unconsciousness or increased reward-related drives, are often caused following subservience to the “emotional brain” as well as by weaker activity of the executive functioning and the forebrain—the “thinking brain,” and are associated with disadvantageous decision-making and risk behaviors. In people with obesity and those with ADHD, the rewarding/hedonic aspects of food items is reflected in a higher insular activity and stronger connections to other reward-related areas [48]. Moreover, individuals with BED, showed lower executive functioning, higher variability in reaction times, and less adaptive response, when compared with otherwise healthy individuals with obesity [49]. Individuals in this group may commonly have excessive body weight.
At the right side of this group are those who eat normally with spontaneous management and no effortful control (B). This small group eats instinctively when they are hungry, chooses foods that satisfy them, enjoys their eating, and stops when they are full or satisfied. They successfully manage to balance between their internal desires and their appetite, eating behaviors, and weight status. They have a spontaneous balance between the emotional and thinking brain and do not need to operate effortful control. Individuals in this group may commonly have stable, normal weight or be slightly overweight. In Western society, only a handful of people fall into this group. The reward signals tend to override the satiety signals; thus, most people’s homeostasis fails in maintaining this balance, with no effort on their part.
Most of the Western population belong to the middle group (C). People in this group assimilate the need to stay healthy, with a stable weight. To achieve this, they apply effortful control and moderate self-discipline. They make sure their diet contains the right amount of nutrients for healthy functioning, and avoid being hungry, and they eat until they are satisfied (although they can eat more). Sometimes, after eating more than they usually do, they balance their eating by sensible restriction or increased physical activity. Their behavior reflects their reasonable decision-making with adequate forethought, indicating adequate prefrontal cognitive control. Food and weight do not control their lives [50]. Their weight may have small fluctuations or stay stable, and they may have a normal weight or may be slightly overweight.
People in the two right groups present dietary restrictions and high abstinence (D and E). Some are ‘weight-watchers’ who show stronger frontal activation than lean subjects in response to food stimuli [51]. They apply chronic, mild to severe restrictions, consume “healthy foods”, stick to low-energy and low-fat diets, and usually follow consistent to rigid eating and physical activity patterns. Many have lost weight and strive to maintain these achievements. Often, maintaining the suppressed weight utilizes high effortful control and may cause lapses and relapses from the rigid diet. Braver et al. suggested that this group activate a proactive-control mode via activation of the prefrontal cortex [52]. They report on early selection of goal-relevant information that is actively maintained in a sustained/anticipatory manner and distracts the individual from their targeted values, perception, and goal-driven action systems. These people may be in a chronic alert status about their weight with different intensities. Their weight status is commonly normal or overweight but still suppressed (D).
The people in the distant right group (E), exhibit rigid to compulsive eating and activity habits because of their emotional brain over-riding their prefrontal brain. Consequently, they activate overcontrol and are undernourished. Many present an anxious temperament (tendency to over responsiveness of cortisol levels), high harm avoidance, and altered reward circuits. People AN or with orthorexia fall in this group; they tend to exhibit obsessive compulsive thoughts and behaviors. It has been hypothesized that anxious traits with abnormalities in the reward circuits could contribute to specific brain pathophysiology and drive extremes of food restriction [53]. For some, the eating disorder is a result of an extremely restricting form of eating and/or compulsive exercising as a means to self-regulate and to achieve a sense of general control, or as part of the extreme pursuit of thinness, which usually reflects projections of control and security issues regarding food and weight.
The goal of this manuscript is to provide an integrative background for the association between large spectrum of eating disorders and the following dimensions: self-regulation, self-control, mentalization, and self-agency, and to justify the need for eating-related mentalization instruments. To bridge the gap between theory and practice, the paper provides an example of a newly developed mentalization tool, to enhance individual self-agency in the management of eating disorders.
As discussed, difficulties in managing negative emotions and negative urgency are transdiagnostic risk factors in a variety of psychological disorders, including EDs. Although the behavioral manifestations of these characteristics may oscillate, the core psychopathology is expressed in the relative balance of under-control and over-control and its effect on body weight, due to fear of losing self-control or due to rigidity (“things must be only my way”). The transition between syndromes and stages of control are associated with changes in the structural functions of the brain’s reward mechanism and the balance between the “emotional brain” and the “thinking brain,” which contribute to reward and anxiety processing, and thus, predispose an individual to eating alternations [53].
Clarifying terminology in psychological science has been recently increasingly emphasized [54,55,56]. Conceptualizing eating and control behaviors on a continuous axis aims to improve the mentalization process and self-agency of people with destructive decisions and behaviors that are associated with eating. The consolidation of eating and control behaviors on the same axis reflects the dialectical nature of decision-making regarding eating in an abundant society. It also presents the dialectic ideas behind Dialectical Behavioral Therapy. The presented eating and control styles axis (ECOSA) may be useful for clinicians who are treating people with EDs as well as other obsessive-compulsive behaviors.
The contribution of the current tool should be rigorously examined in a randomized clinical trial. Future research may want to assess the validity of this tool by comparing mentalization-based therapy using the ECOSA with, mentalization-based treatment without the ECOSA and see if this tool has an effect on treatment outcome.
Despite this drawback, the developed tool can be used by professionals to promote individual’s mentalization by clarifying terminology, assist the clients to differentiate between under and over control as well as understand the mediating thinking patterns and brain areas contributing to their extreme behaviors. This tool may assist individuals in understanding the complexity that underlined their symptoms, improve their self-agency and treatment objectives, as well as increase their sense of effectiveness and motivation to challenge the negative defense mechanisms.
The authors have no conflicts to disclose
Both authors contributed to the writing of this manuscript.
No Funding
- Cella, S., Iannaccone, M., Cipriano, A., and Cotrufo, P. (2020) Risk and maintenance factors for eating disorders: An exploration of multivariate models on clinical and non-clinical populations. IntechOpen. Advance online publication. DOI: 10.5772/intechopen.91063
- Aldao, A., Nolen-Hoeksema, S., and Schweizer, S. (2010) Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review 30: 217–237. https://doi.org/10.1016/j.cpr.2009.11.004).
- Lukas, C. A., Ebert, D. D., Fuentes H. T., Caspar, F., Berking M., Pedersen, S. H. , Lunn, S. , Katznelson, H., and Poulsen, S. (2012) Deficits in general emotion regulation skills–Evidence of a transdiagnostic factor. European Eating Disorders Reviews 20(4): 303–310.
- Mallorquí-Bagué, N., Vintró-Alcaraz, C., and Sánchez, I., et al. (2018). Emotion regulation as a transdiagnostic feature among eating disorders: cross-sectional and longitudinal approach. European Eating Disorders Review 26(1): 53–61. doi:10.1002/erv.2570
- Baumeister, R. F., Gailliot, M., DeWall, C. N. and Oaten, M. (2006) Self-regulation and personality: How interventions increase regulatory success, and how depletion moderates the effects of traits on behavior. Journal of Personality 74: 1773–1801.
- Muraven, M., Shmueli, D., and Burkley, E. (2006) Conserving self-control strength. Journal of Personality and Social Psychology 91: 524–537.
- Juarascio, A., Lantz, E. L., Muratore, A. F., and Lowe, M. R. (2018) Addressing Weight Suppression to Improve Treatment Outcome for Bulimia Nervosa. Cognitive and Behavioral Practice 25(3): 391–401. https://doi. org/10.1016/j.cbpra.2017.09.004
- Kaplan, A. S., & Strober, M. (2019) Severe and enduring anorexia nervosa: Can risk of persisting illness be identified, and prevented, in young patients? Int J Eat Disord 52(4): 478–480. https://doi.org/10.1002/eat.23019
- Jewell, T., Collyer, H., Gardner, T., Tchanturia, K., Simic, M., Fonagy, P., and Eisler, I. (2016) Attachment and mentalization and their association with child and adolescent eating pathology: A systematic review. International Journal of Eating Disorders 49(4): 354–373.
- Bateman, A. W., and Fonagy, P. (2006) Mentalization-based treatment for borderline personality disorder. Oxford: University Press.
- Bleiberg, E. (2004) Treating personality disorders in children and adolescents: A relational approach. New York, N.Y.: Guilford Press.
- Weinberg, E. (2006). Mentalization, affect regulation, and development of the self. Journal of the American Psychoanalytic Association 54(1): 251–269. https://doi. org/10.1177/ 00030651060540012501(8) | Request PDF. (n.d.). Retrieved 13 March 2020, from https://www. researchgate.net/publication/222420066_Impulsivity-related_traits_in_eating_disorder_patients
- Scherer, K. R. (2005) What are emotions? And how can they be measured? Social Science Information 44: 695– 729. doi:10.1177/053901840505821
- Tamir, M. (2016). Why do people regulate their emotions? A taxonomy of motives in emotion regulation. Personality and Social Psychology Review 20: 199–222. http://dx.doi. org/10.1177/1088868315586325
- Mauss, I. B., Bunge, S. A., and Gross, J. J. (2007) Automatic emotion regulation. Social and Personality Psychology Compass 1: 146–167. doi:10.1111/j.1751- 9004.2007.00005.x
- Reiss, S., Peterson, D.M., Gursky, M., McNally R. (1986) Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Journal of Behavoral Research Therpies 24(1): 1–8.
- Schmidt, N. B., Zvolensky, M. J., and Maner, J. K. (2006) Anxiety sensitivity: Prospective prediction of panic attacks and axis i pathology. Journal of Psychiatric Research 40: 691–699. https://doi.org/10.1016/j. jpsychires.2006.07.009.
- Juarascio, A., Manasse, S., Clark, K. E., Schaumberg, K., Kerrigan, S., Goldstein, S. P., and Forman, E. (2020) Understanding the overlap and differences in terms describing patterns of maladaptive avoidance and intolerance of negative emotional states. Personality and Individual Differences. Elsevier Ltd. https://doi. org/10.1016/j.paid.2020. 109859.
- Fischer, S., and Munsch, S. (2012) Self-regulation in eating disorders and obesity—implications for treatment. Verhaltenstherapie 22: 158– 164. https ://doi. org/10.1159/00034 1540
- Slade, P. (1982) Towards a functional analysis of anorexia nervosa and bulimia nervosa. British Journal of Clinical Psychology 21: 167–179.
- Haynos, A. F., Wang, S. B., and Fruzzetti, A. E. (2018) Restrictive eating is associated with emotion regulation difficulties in a non-clinical sample. Eating disorders 26(1): 5–12. https://doi.org/10.1080/10640266.2018.141 8264
- Gratz, K. L., and Roemer, L.(2004) Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment 26: 41–54. https://doi.org/10.1023/B:JOBA.0000007455.08539.94.
- Williams-Kerver, G. A., and Crowther, J. H. (2020) Emotion differentiation and disordered eating behaviors: The role of appearance schemas. Eating Behaviors 37: 101369. DOI: 10.1016/j.eatbeh.2020.101369
- Anestis, M. D., Selby, E. A., Fink, E. L., and Joiner, T. E. (2007) The multifaceted role of distress tolerance in dysregulated eating behaviors. International Journal of Eating Disorders 40: 718–726. doi:10.1002/eat.20471.
- Culbert K.,M, Racine, S.E, Klump, K.L. (2015) Research Review: What we have learned about the causes of eating disorders – A synthesis of sociocultural, psychological, and biological research. Journal of Child Psychology and Psychiatry 56(11): 1141–1164.
- Vander Broek-Stice, L., Stojek, M. K., Beach, S. R. H., van Dellen, M. R., and MacKillop, J. (2017) Multidimensional assessment of impulsivity in relation to obesity and food addiction. Appetite 112: 59 –66.
- Langer, M., Bord, A., and Golan, M. (2015) Differences in impulsivity between females diagnosed with eating disorders and healthy subjects. J Psychology and Clinical Psychiatry 3(3): 0013.
- Trafton, J. A., and Gifford, E. V. (2011) Biological bases of distress tolerance. In: Zvolensky, M. J, Bernstein, A, Vujanovic, A. A., Editors. Distress Tolerance. New York: Guilford Press.
- Steward, T., Mestre-Bach, G., Vintró-Alcaraz, C., Agüera, Z., Jiménez-Murcia, S., Granero, R., and Fernández- Aranda, F. (2017) Delay Discounting of Reward and Impulsivity in Eating Disorders: From Anorexia Nervosa to Binge Eating Disorder. European Eating Disorders Review. https://doi.org/10.1002/erv.2543
- Bohon, C., and Stice, E. (2012) Negative affect and neural response to palatable food intake in bulimia nervosa. Appetite 58: 964–970.
- Eyden, J., Winsper, C., Wolke, D., Broome, M.R.and MacCallum, F. (2016) A systematic review of the parenting and outcomes experienced by offspring of mothers with borderline personality pathology: Potential mechanisms and clinical implications. Clinical Psychology Review 47: 85-105. DOI: 10.1016/j.cpr.2016.04.002.
- Fonagy, P., Gergely, G., Jurist, E. L., and Target, M. (2018) Affect regulation, mentalization and the development of the self. Affect Regulation, Mentalization and the Development of the Self. https://doi.org/10.4324/9780429471643
- Skårderud, F., and Fonagy, P. (2012) Eating disorders. In A. Bateman, and P. Fonagy (Eds.), Handbook of mentalizing in mental health practice. Washington, D. C: American Psychiatric Puhlishing, Inc. pp. 347–384.
- Rothschild-Yakar, L., Waniel, A.and Stein, D. (2013) Mentalizing in self vs. parent representations and working models of parents as risk and protective factors from distress and eating disorders. Journal of Nervous and mental Diseases 201: 510–518.
- Skårderud, F. (2007) Eating one’s words, part I: ‘Concretised metaphors’ and reflective function in anorexia nervosa–an interview study. European Journal of Eating Disorders Review 15: 163–174. 10.1002/erv.777
- Harrison, A., Tchanturia, K., and Treasure, J. (2010) Attentional bias, emotion recognition, and emotion regulation in anorexia: state or trait? Biological Psychiatry 68(8): 755–761
- Sacchetti, S., Robinson, P., Bogaardt, A., Clare, A., Ouellet-Courtois, C., Luyten, P.and Fonagy, P. (2019). Reduced mentalizing in patients with bulimia nervosa and features of borderline personality disorder: A case-control study. BMC Psychiatry 19(1): 1–12. https://doi. org/10.1186/s12888-019-2112-9
- Tasca, G. A., Demidenko, N., Krysanski, V., Bissada, H., Illing, V., Gick, M., et al. (2009a) Personality dimension among women with an eating disorders: Towards reconceptualizing DSM. European Eating Disorders Review 17: 281–289. 10.1002/erv.938.
- Lavender, J. M., Wonderlich, S. A., Engel, S. G., Gordon, K. H., Kaye, W. H., and Mitchell, J. E. (2015b) Dimensions of emotion dysregulation in anorexia nervosa and bulimia nervosa: A conceptual review of the empirical literature. Clinical Psychology Review 40: 111–122. https://doi. org/10.1016/j.cpr.2015.05.010.).
- Bateman, A. W., and Fonagy, P. (2012) Individual techniques of the basic model. Handbook of Mentalizing in Mental Health Practice 67–80.
- Haggard, P., and Tsakiris, M. (2009) The experience of agency feelings, judgments, and responsibility. Current Direction in Psychological Science 18: 242–246. 10.1111/j.1467-8721.2009.01644.x
- Nahab, F.B., Kundu1, P., Gallea, C., Kakareka, J., Pursley, R., Pohida, T., et al. (2011) The neural processes underlying self-agency. Cerebral Cortex 21: 48-55 doi:10.1093/ cercor/bhq059.
- Fonagy P., Luyten P., Moulton-Perkins A., Lee Y.W., Warren F., Howard S. and Lowyck, B. (2016) Development and validation of a self-report measure of mentalizing: The Reflective Functioning Questionnaire. Plos One 11(7): 0158678. doi: 10.1371/journal.pone.0158678
- William, D., and Lewitt, H. (2007) Principles for facilitating agency in psychotherapy. Psychotherapy Research 17(1): 66–82.
- Fonagy, P., and Bateman, P. (2012) Eating disorders. In A. Bateman, and P. Fonagy (Eds.), Handbook of mentalizing in mental health practice. Washington, D. C: American Psychiatric Publishing, Inc. pp. 347–384.
- Leventhal, H., Brissette, I., Leventhal, E. A., and Cameron, L. D. (2003) The common-sense model of self-regulation of health and illness. The Self-Regulation of Health and Illness Behaviour, London, Routledge pg. 42-65.
- Robinson, P., Hellier, J., Barrett, B., Barzdaitiene, D., Bateman, A., Bogaardt, A., Clare, A., Somers, N., O’Callaghan, A., Goldsmith, K., Kern, N., Schmidt, U., Morando, S., Ouellet-Courtois, C., Roberts, A., Skårderud, F.and Fonagy, P. (2016) The NOURISHED randomised controlled trial comparing mentalisation-based treatment for eating disorders (MBT-ED) with specialist supportive clinical management (SSCM-ED) for patients with eating disorders and symptoms of borderline personality disorder. Trials 17(1): 549–564.
- Munsch, S., Dremmel, D., Wilhelm, P., Baierlé, S., Fischer, S., and Hilbert, A. (2019) To eat or not to eat: reward delay impulsivity in children with loss of control eating, attention deficit / hyperactivity disorder, a double diagnosis, and healthy children. PLoS One 14(9): e0221814.
- Blume, M., Schmidt, R., and Hilbert, A. (2018) Executive Functioning in Obesity, Food Addiction, and Binge-Eating Disorder. Nutrients 11(1): 54. https://doi.org/10.3390/ nu11010054
- Davidson, T. L., Jones, S., Roy, M., and Stevenson, R. J. (2019) The cognitive control of eating and body weight: it is more than what you “think”. Frontier in Psychology, 13: https://doi.org/10.3389/fpsyg.2019.00062
- Sweet, L. H., Hassenstab, J. J., Mccaffery, J. M., Raynor, H. A., Bond, D. S. Demos K. E., et al. (2012) Brain response to food stimulation in obese, normal weight, and successful weight loss maintainers. Obesity (Silver Spring) 20: 2220–2225 10.1038/oby.2012.125
- Braver, T. S., Paxton, J. L., Locke, H. S., and Barch, D. M. (2009) Flexible neural mechanisms of cognitive control within human prefrontal cortex. Proceedings of the National Academy of Sciences of the United States of America 106(18): 7351–7356. https://doi.org/10.1073/ pnas.0808187106.
- Frank, G. K. W., DeGuzmana, M. C., Megan, E., and Shott, M. E. (2019) Motivation to eat and not to eat – The psycho-biological conflict in anorexia nervosa. Physiology and Behavior 206: 185–190.
- Lilienfeld, S. O., Pydych, A. L., Lynn, S. J., Latzman, R. D., and Waldman, I. D. (2017) Fifty differences that make a difference: A compendium of frequently confused term pairs in psychology. Frontiers in Education https://doi.org/10.3389/feduc.2017.00037.
- Engel, S. G., Wonderlich, S. A., Crosby, R. D., Mitchell, J. E., Crow, S.and Peterson, C. B., et al.(2013) The role of affect in the maintenance of anorexia nervosa: Evidence from a naturalistic assessment of momentary behaviors and emotion. J Abnorm Psychol 122: 709–719. [PubMed: 24016011]
- Pederson, S,H., Lunn S., Katznelson, H. (2012) Reflective Functioning in 70 Patients Suffering from Bulimia Nervosa. European Eating Disorders Review 20(4): 303- 310. doi: 10.1002/erv.2158%0D.













