Article / Research Article
First Year MPH Student, UC Berkeley, United States.
Brook Lyn Mercado
First Year MPH Student,
UC Berkeley,
United States.
6 February 2024 ; 21 February 2024
The people of the United States territories have faced healthcare inequalities for years due to ongoing, complex issues with their public health infrastructure. During the 2009 influenza pandemic, the U.S. territories faced several dilemmas such as insufficient funding, a lack of laboratory equipment, personal protective equipment, and surveillance to predict the spread of the disease, due to the ongoing health disparities and complications with their public health infrastructure (Dopson, 2016). These patterns have also been seen during the COVID-19 pandemic in addition to new dilemmas such as damaged physical public health infrastructure. The objective of this research was to compare and contrast the effects of COVID-19 in the U.S. territories to the U.S. while examining the social and cultural conditions of these territories. A descriptive analysis of data on covid mortality rates and vaccination rates has been completed showing that disparities did occur throughout the pandemic. These dependent variables were explored for all of the U.S. territories and thoroughly compared to one another to make a descriptive assessment of the vaccination and mortality outcomes. Relevant social and cultural conditions were examined as well (i.e. effects on infrastructure from natural disasters, and policies in place during the pandemic). Conclusions about these outcomes within the territories have allowed us to recognize distinct patterns from the latest data available. There are differences in how these disparities occur in the U.S. territories and how COVID-19 has affected them. Through this study, there have been new themes seen throughout the pandemic such as a sense of community and support, geographic isolation, and politics that may have contributed to the vaccination rates and mortality rates seen in these territories. The implications of this study push for future research to be completed as casual analyses were not completed and should be looked at moving forward.
The coronavirus disease, COVID-19, has taken the lives of approximately 6,125,095 people (World Health Organization (WHO) July 19, 2022) and continues to do so. Several countries were ill-prepared to handle such a large-scale and highly contagious infectious disease, creating many challenges worldwide when it came to disease prevention and slowing the spread of disease. The impact of the COVID-19 pandemic led to drastic changes in everyday life on a global scale, which exacerbated disruption to one’s routine. During the pandemic, restrictions were placed on travel, masks were required, and virtual or remote arrangements were implemented to limit face-to-face interaction. Early in the pandemic, most of the world limited business operations by requiring early closures as well as entirely shutting down nonessential businesses which in turn led to lost jobs and more economic hardships. While many of these changes were universal, the impacts they had on different groups of people varied.
The objective of this research is to compare and contrast the effects of the COVID-19 pandemic in the United States territories to the United States while exploring health disparities related to the territories’ social and cultural conditions. Effects of COVID-19 in the United States territories is a story untold and not focused on often through media and overall research. The U.S. territories have a long history of dealing with health disparities that often go overlooked and are deemed irrelevant to and separate from the United States. U.S. territories are not countries or states, but rather land acquired by the United States. Each U.S. territory has its own government; however, the U.S. Congress has every legal right to make “all needful rules and regulations respecting the territory” (Government Accountability Office, [GAO], 1991). Even though the United States and its territories have very complex relationships, there are healthcare inequalities that are faced by the people of each of these locations.
Healthcare inequalities are rooted in systematic oppression for those who have low income, lack higher education, live in rural communities, are members of the LGBTQ+ community, are women, are racially or ethnically marginalized, and more. These inequalities can lead to disparities in healthcare outcomes such as vaccination rates, mortality rates, and total number of cases of a disease. Health disparities discussing race, social-economic status, and rural vs urban have been thoroughly researched in the United States; however, literature is lacking on these determinants of health among the U.S. territories. In this study, social and cultural conditions will be examined in order to explore the health disparities that have impacted the U.S. territories during the COVID- 19 pandemic. It is important to discuss the pandemic’s effects in the U.S. territories not only because it is not discussed enough, but because they have limited resources, funding, and overall support from the United States. The United States has been trying to reduce healthcare inequalities within the states, but it is time that goal also focusses on helping the U.S. territories as well.
This thesis aims to explore the impact of the ongoing COVID-19 in the U.S. territories by conducting a descriptive analysis utilizing data regarding COVID-19 vaccination rates and mortality rates from the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) in conjunction with information about social and cultural conditions within specific U.S. territories that provide context for the data explored. By making causal associations with the data and social and cultural conditions, assumptions can be made as to if the U.S. territories had adequate support during the COVID-19 pandemic from the United States as well as if anything was successful in mitigating the impact of COVID-19. There are lessons to be learned by looking at this information and making connections, which will be discussed.
COVID-19
The novel coronavirus disease (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Following its discovery in Wuhan, China, in November 2019, COVID-19 spread globally including in the United States, where the first confirmed case was documented in January 2020 (CDC, 2022). This disease activates mild to severe symptoms of illness within 2-14 days of exposure that resemble respiratory responses (i.e., cold, flu, and pneumonia) (CDC, 2022, 2021). It can also lead to potentially fatal responses like increased susceptibility to infections by microorganisms, septic shock, and multiple organ failure (Yang et. al., 2020).
COVID-19 is spread via droplets and particles from one infected person to another. The known methods of transmission from an infected person include the following:
- Breathing in air when in close proximity;
- Contact with the eyes, mouth, or nose from a cough or sneeze;
- Contact with the eyes, mouth, or nose when touched by hands contaminated with the virus (CDC, 2021).
When the pandemic began on January 20, 2022, there was a lot of confusion and misinformation about COVID-19. Many people were frightened, and society saw the effects almost immediately. Mask mandates and social distancing spread nationwide creating political tension. Schools and jobs changed the format to remote in order to prevent the spread of COVID-19. This continued for over a year, uprooting the lives of many. In December 2020, the first person in the United States, outside of a clinical trial, was vaccinated, which began a new phase of the pandemic in which preventative public health measures included incentives to vaccinate as many people as possible. This began with money offers from a large lottery to $25 at one’s place of employment, free food from restaurants, and even free tuition lotteries. Even though this was progress towards a future free of COVID-19, the pandemic was far from over, and the long-term psychological and physiological effects of the pandemic are still in question. In August 2022, many places still required masks and some places required individuals to provide proof of vaccination. There are continuous spikes of COVID-19, and there is a growing view that this disease might not ever go away becoming an endemic like the flu (Feldscher K., 2021). Publicized information in media regarding the specific impacts of COVID-19 in the U.S. territories has been limited within the United States.
The United States consists of 50 states and 5 territories. A United States territory is defined as a jurisdiction that is neither a part of one of the several States nor a Federal district (16 USC § 6602(9)). Each state has its own laws and regulations and has different needs and expectations when it comes to healthcare. The U.S. territories are directly controlled by the federal government of the United States. Each territory is allowed to have its own government to manage local affairs. Each territory also has a non-voting member within the U.S. House of Representatives, similarly to the District of Columbia. Since the territories lack sovereignty, they ultimately lack the same rights as the states within the United States even though all individuals born in a U.S. territory are U.S. citizens, except for those in American Samoa who are considered U.S. Nationals. There are five populated U.S. territories: American Samoa, Guam, the Northern Mariana Islands otherwise known as the Commonwealth of the Northern Mariana Islands (CNMI), Puerto Rico, and the U.S. Virgin Islands (USVI). Hereafter, the Northern Mariana Islands will be referred to as CNMI, and the U.S. Virgin Islands will be referred to as USVI. The locations of each territory as described can be seen in Figure 1. Puerto Rico (Red) and the U.S. Virgin Islands (Orange) are located in the Caribbean Sea in the Atlantic Ocean. Guam (Green) and the Northern Mariana Islands (Purple) are located in the North Pacific Ocean. American Samoa (Yellow) is located in the South Pacific Ocean.
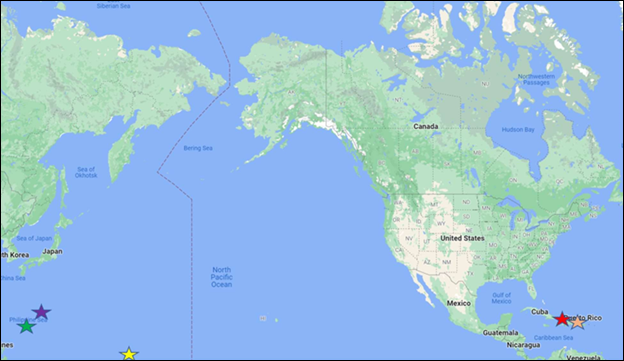 Figure 1: Map Demonstrating Locations of the Territories of the United States
Figure 1: Map Demonstrating Locations of the Territories of the United States
The United States and the U.S. territories have complex relationships that contribute to the ongoing health disparities that occur within these territories. These individual entities all have their own similarities and differences with one another in regard to government structure, health care systems, and the way COVID-19 was handled. These differences have led to contrasting health outcomes from the recent pandemic which will be explored in this project.
Health disparities have contributed to the different patterns seen in COVID-19 outcomes, including vaccination rates and mortality rates, within the United States and within the U.S. territories. Health disparities are defined as preventable differences in the burden of disease, injury, violence, or opportunities to achieve optimal health in society that are experienced deleteriously by socially disadvantaged populations (CDC, 2020). According to this definition, some groups in society experience systematic disadvantages when it comes to both impacts of disease and access to health promoting and illness preventing resources. Both kinds of systematic disadvantages comprise health disparities. Social risk factors that drive health disparities include but are not limited to race, ethnicity, gender, education, economic status, disability, geographic location, and sexual orientation, statuses that interact with each other as well as the environments where people work, live, learn, and play (Link & Phelan, 1995). In sum, these social determinants of health or social conditions are considered by social epidemiologists as fundamental causes of disease, as systems of poverty, racism, sexism, and more are empirically established root causes of health disparities (Link & Phelan, 1995). These determinants are categorized into five key areas that influence health:
- economic stability
- education access and quality
- healthcare access and quality
- neighborhood and environment
- social or communal context (CDC, 2021)
This project includes descriptive exploration of three of these five key areas – healthcare access and quality, social or communal context, and environment – which are explored in more depth in the following subsections.
Access to healthcare is the ability to receive healthcare services. It consists of four components: coverage, services, timeliness, and workforce. Quality of care is the measure of which healthcare resources provide and has been an ongoing issue within the U.S. territories. In 2011, a study was done to compare the quality of care within the United States and the U.S. territories (Nunez-Smith, et al, 2011). The conclusion of this study found that the quality of care in the U.S. territories is not up to par with the United States. Due to the lack of influence the U.S. territories have on their own healthcare policies, there needs to be change moving forward to better support the territory’s healthcare needs. Access to healthcare as well as quality of care have lasting impacts on the health outcomes of COVID-19.
Access to healthcare within rural and more remote areas can be a challenge that many people face, especially those within the U.S. territories. Sometimes, patients within the territories may need to receive care for more complex health issues in the United States due to the lack of resources. Before CNMI built an oncology center on site, they were sending nearly 300 patients a year to receive care in Hawaii (Stolyer et al, 2021).
Similar limitations are seen throughout the COVID-19 pandemic specifically in regard to testing for COVID-19. In March of 2020, Puerto Rico and Guam were the only U.S. territories able to test for COVID-19 in public labs (Georgieve and Kaplan, 2020). All other U.S. territories had to ship their tests to Hawaii who had specific requirements that needed to be met in order to receive a COVID-19 test. If a patient did not meet Hawaii’s testing criteria, their specimen would then be sent to Atlanta, Georgia further delaying the results, and ultimately affecting data collection. Even though Puerto Rico had public labs for testing, during spring of 2020, they had the lowest per-capita testing rates compared to any state due to lack of supplies (Coto, 2020). Only 15 COVID tests were being done every day per 100,000 people. This was an issue because the data that was being collected early in the pandemic was inaccurate as far as the number of cases. The number of COVID-19 tests administered was also inaccurate at the beginning of the pandemic in Puerto Rico due to people who were being tested getting counted twice initially in case counts, once for a nasal swab, and once for a blood test (Mazzei, 2020). Tests were also given out extremely slowly within the U.S. territories. Another delay patients faced is they would have to test negative for flu and bacterial pneumonia before being given a COVID-19 test, furthering the delay for results (Mazzei, 2020).
In the United States, tests were and are accessible to most people. Some limitations to access testing were location and lack of tests in a particular area. If you showed any COVID-19 symptoms, such as a sore throat, loss of taste or smell, or had been in contact with somebody who tested positive for COVID-19, you would have better luck finding access to a test. There were also mass testing opportunities in populated areas as well as free tests shipped directly to people’s homes in early 2022. As of September 2022, COVID-19 tests can be purchased at retailers and online.
In addition to testing limitations, there were also issues with the U.S. territories having an adequate number of staff to conduct tests. Most U.S. territories lacked the staff to administer COVID-19 tests (Gilbert, 2020) early in the pandemic. The U.S. territories lose many doctors and nurses every year to the states because of their lack of resources, lack of funding, and working conditions increasing the lack of access to care. From 2005 to 2013, 12% of Puerto Rico’s physicians and surgeons left for the United States (Patron, 2017) due to unmanageable amounts of patients, and the United States offering better salaries, working conditions, and resources. Health care workers in the U.S. territories continue to leave for the United States seeking better opportunities to provide care. The COVID-19 pandemic also contributed to the loss of healthcare staff within both the United States and the U.S. territories. This was due to many healthcare workers struggling to keep up with the demand and dissatisfaction with their pay leading to high turnover rates (Ollove, 2022). Without adequate staffing to combat COVID-19, access to appropriate care for many people was limited.
Vaccination distribution began in the United States as well as within the U.S. territories with the prioritization of high-risk individuals as well as health care workers. Over time, vaccinations became more readily available to the public. The Food and Drug Administration (FDA) initially approved each COVID-19 vaccination for emergency use beginning with adults, followed by those age 12 to 17, then 5 to 11, and finally those 6 months and over. As of October 2022, the Pfizer vaccine and Moderna vaccine are fully FDA approved. COVID-19 vaccinations are free within both the United States and all of the U.S. territories. In the United States, vaccinations were available throughout the country not long after the first American was vaccinated against COVID-19 in December 2020. Availability was limited to those who needed it most such as healthcare workers, those 65 and older, and high-risk individuals. Demand for the initial COVID-19 vaccines varied from state to state as did how they were made available to the general public. By summer 2021, vaccination roll out began to open to all adults once initial demand was met.
The U.S. Army and National guard were vital in assisting the U.S. territories and several stated in COVID-19 vaccination distribution. Twelve U.S. Army medical staff members were placed on CNMI for a 30-day campaign to assist in vaccinating the community (Joint Region Marianas Public Affairs, 2021). U.S. Army medical professionals were also placed in Guam to help administer vaccinations (Weissman, 2021). Puerto Rico received assistance from the U.S. National Guard to distribute vaccinations (Steinhauer, 2021). In total, 16 states and U.S. territories received assistance from the U.S. National Guard for vaccine distribution (Steinhauer, 2021). Puerto Rico was determined to make sure vaccines could be accessed even within the most rural areas of the island. The CDC helped train 1,000 healthcare providers to be informed about the vaccine and the Puerto Rico Department of Health (PRDH) helped train another 20,000 providers (Steinhauer, 2021). The CDC, PRDH, and Immunization Program worked together to quickly get vaccinations to providers all over the island, as well as create strategies to swiftly educate those providers to educate the public. Puerto Rico held several vaccination events and even went as far as to go to church services, beaches, and even bars to offer the vaccine. The U.S. Army and National Guard were essential in vaccinating the U.S. territories as well as the states. Although these territories were able to provide vaccinations to their communities, they did so while facing challenges that were uncommon within the United States.
The U.S. territories followed stricter practices in order to mitigate the spread of COVID-19 compared to the United States. Part of this was because COVID-19 was not considered a political issue but rather a health issue in the territories. In the United States, the individual is more valued than the community. COVID-19 vaccinations became a political issue, public health measures were criticized for their infringements on individuals, and science and data about the pandemic were villainized. The U.S. territories had a different experience and approach to the pandemic in these regards, that of course not everybody agreed with, however, within the U.S. territories people were able to come together for a common goal. The U.S. territories placed a high value on the community over the individual, and that showed in their practices to mitigate the spread of COVID-19.
Public policies are an area in which there were some similarities and key differences between the United States and U.S. territories. One major area of policy that is key to examining the outcomes of the COVID-19 pandemic are policies pertaining to travel bans and border closures. The Unites States Affiliated Pacific Islands (USAPI) began early travel bans. American Samoa completely closed its borders in March of 2020, and CNMI closed its borders in April of 2020. The USAPI heightened surveillance and testing requirements within the region which included multiple tests during quarantine and enhanced contact tracing. Guam closed schools the day after the first case of COVID-19 on the island was announced. Similar practices that were implemented within the United States such as mask mandates and capacity limits were also done in all of the U.S. territories. The USAPI worked together toward a common goal of mitigating the spread of COVID-19 supporting one another which ultimately led to better health outcomes compared to the United States. USVI also implemented similar policies of mask mandates, curfews, and testing requirements for travel. Although similar policies were followed across the United States and U.S territories, there were some limitations regarding guidelines in some territories.
One dilemma Puerto Rico faced is that its border never really closed. Although international flights were limited for some time, domestic flights were still coming and going to the territories. Tourists from the United States continued to vacation in Puerto Rico. It was reported that tourists had a lack or regard for the COVID-19 mask mandates, curfews, and other safety precautions (Acevedo, 2021). Since the U.S. territories are technically a part of the United States, flights to and from the territories to the United States are considered domestic. This allowed tourists from the United States to go to and from while following all federal guidelines. Tourism was in fact the cause of Puerto Rico’s first COVID-19 case. According to ABC News, Puerto Rico’s first COVID-19 case actually was an Italian tourist who visited Puerto Rico on a cruise (2020). Following this, Puerto Rico enacted strict curfews from 10:00 PM to 5:00 AM, and citizens were faced with legal action if the new rules were not followed. Many sources actually stated that the prime source of contagion in Puerto Rico was the Luis Muñoz Marín International Airport (Rodríguez Velázquez & Colón Almena, 2020). According to Wanda Ortiz, president of the Puerto Rico Association of Epidemiologists, flights should have been halted from the beginning to avoid the spread of COVID-19 during the early stages of the pandemic (2020) which is exactly what American Samoa did.
American Samoa closed its borders in March 2020 and began repatriation flights, flights organized by the government to bring citizens home, in this case to American Samoa, in January 2021 (Richardson, 2021). This was successful in keeping COVID-19 out of the territory temporarily. American Samoa was free of COVID-19 until September 17, 2021. The positive case was brought to American Samoa by a resident who was returning from Hawaii on a repatriation flight. The passenger had caught the very first flight back since travel restrictions began back in March 2020 (Firozi & Shammas, 2021). Upon discovering the passenger was positive, three days after arriving on the island, future flights were postponed. Those coming into American Samoa on repatriation flights had to test negative before flying and then get tested again upon arrival, which is how their first case was caught early on to avoid community spread. American Samoa had its first community-transmitted case of COVID-19 this year, 2022, in March. The island was placed under a state of emergency and all nonessential businesses were closed and a nationwide lockdown ensued. Before this case, all others had tested positive while in quarantine and no deaths had yet occurred (Westerman, 2022). Limiting travel and taking necessary precautions such as masks seem to have helped in one way or another within each territory and within the United States, however, there were other policy factors that contributed to the outcomes of the COVID-19 pandemic.
Each U.S. territory had their own unique dilemmas throughout the pandemic.
Puerto Rico faced challenges regarding leadership and public health management. Since the beginning of the COVID-19 pandemic, December 2019, there were 4 secretaries of health in Puerto Rico. Two of them left their position within the first 3 months, one lasting as short as two weeks. Their lead epidemiologist also resigned 3 months into the pandemic (Serrano-Roman, 2020). This delayed community preparedness as community members were being given misleading information regarding the pandemic from the lead epidemiologist. The consistent changes amongst the secretaries of public health also caused disarray as this increased lack of communication. Guam also faced a unique challenge unlike the other U.S. territories. On March 7th, 2020, the USS Theodore Roosevelt, a military aircraft carrier, docked on the island of Guam. The ship hosted approximately 4800 sailors. After an event in Vietnam, sailors began to test positive for COVID-19 prior to docking in Guam. The situation got worse, and 4,000 hotel rooms were booked on the island of Guam to house the infected and exposed sailors. In total, 1,271 sailors tested positive for COVID-19 (Kasper et al., 2020). Guam locals protested hosting the sailors and felt that there was a “reckless double-standard” of placing “potentially exposed military personnel in local hotels,” (Senator Sabina Flores Perez, 2020). As of October 2022, there is no information whether the docking of the USS Roosevelt contributed to the spread of COVID-19 on the island or not.
In addition to health policies and other practices that were apparent throughout the pandemic, there are additional social and communal contexts that are relevant when exploring the outcomes of the COVID-19 pandemic. In addition to health policies, healthcare systems and government structures can impact health outcomes. Health outcomes of previous pandemics are also relevant as they can allow us to make comparisons of how the past had affected the present in regard to policy, support, health infrastructure, and preparedness to combat a pandemic. These features will be explored in the following subsections.
Past pandemics can provide insight as to how specific societies were affected and allow for opportunities to better understand the current pandemic which includes an outline of health disparities within the U.S. territories. In 2009, there was an influenza pandemic that rapidly spread throughout the globe. Influenza A (H1N1) is a virus that can cause highly contagious, respiratory illness, the flu. Symptoms of H1N1 include fever, chills, sneezing, coughing, and a sore throat (CDC, 2021). The flu is a seasonal disease caused by different influenza strains and epidemics occur yearly. A pandemic from the flu is rare, as there have only been 4 in the past 100 years (CDC, 2018).
During the 2009 influenza pandemic, the Pacific U.S. territories faced several disadvantages when it came to protecting the communities from this disease. One major limitation in public health infrastructure that they faced was the lack of surveillance resources. From 2006-2007 the Pandemic and All-Hazards Preparedness Act and the CDC provided supplemental influenza pandemic funding to the USAPI. The USAPI is made up of three U.S. territories: Guam, CNMI, and American Samoa in addition to three Freely Associated States – the Republic of Palau, the Republic of the Marshall Islands, and the Federated States of Micronesian. Those who received grants were supposed to be able to conduct year-round electronic surveillance for seasonal influenza, have dedicated ship-to sites for vaccines as well as temperature monitoring and data collections for vaccine administration. Funding was limited and had to be used to enhance current surveillance and laboratory spaces. When the public health emergency was declared in the United States in April of 2009, the USAPI was unprepared for a pandemic. These territories still lacked the ability to survey the population: surveillance was still being done manually. There were no electronic surveillance systems on any Pacific Island, however, the United States exclusively used electronic surveillance systems in place to detect and prevent the spread of H1N1 (Dopson, 2016).
In 2009, during the influenza pandemic, Congress provided funding through H.R. 2346, Supplement Appropriations Act. The funds provided were to address vaccination, epidemiology and laboratory capacity, information technology infrastructure, and general preparedness and planning. USAPI received additional funding from the CDC and Subject Matter Expert assistance with the deployment of CDC personnel throughout the pandemic, which became extremely helpful when it came to delivering vaccines to the population. A total of 28 CDC personnel were deployed to USAPI which consisted of 500,000 people and hundreds of islands and contributed $172,900 in resources. This funding allowed USAPI to expand its laboratories, however, there was still no laboratory in these territories to receive a specimen and analyze it. All specimens, including influenza, had to be shipped to a lab in California, Hawaii, or Texas. Delays from shipping samples can lead to delays in detecting influenza. Funds from the CDC are now used to provide an expert regional laboratory coordinator from the Pacific Islands Health Officer Association to meet with each jurisdiction and provide training yearly (Dopson, 2016).
In addition to these ongoing problems faced, once vaccines were available, they took 7 days to ship from the mainland to USAPI. If all allocated vaccines were shipped at once, there was a challenge of making sure there was enough refrigeration space and backup generators to keep vaccines at the proper temperature. This was extremely limiting to American Samoa as their power was sporadic due to a recent tsunami. Another problem that these territories faced were consent forms for those who wanted to be vaccinated. They had to be translated into local languages. The Supplemental Appropriations Act did assist the USAPI in a multitude of ways paving the way for future goals to be met such as laboratory capacity to obtain and analyze samples, create better surveillance systems, and provide expert training to laboratory staff (Dopson, 2016).
The U.S. healthcare system is composed of public and private, for-profit, and nonprofit insurance companies and healthcare providers. Insurance coverage is dependent on many factors such as age, economic status, employment status, veteran status, disability status, and pregnancy status (Medicaid.gov, 2022). If a person is above the age of 65, they qualify for Medicare, a federally funded health insurance. Unlike Medicaid, an individual may have to pay a monthly premium for this insurance. People may also qualify if they have a certain disability. If an individual is a low-income household, pregnant, is a child, or receives social security income, they may qualify for Medicaid, a federally mandated insurance program that is implemented differently by each state.
Medicaid provides free or low-cost coverage to those who qualify. Those who are employed full-time may be offered insurance through their job under a cost-sharing program. These individuals will pay a monthly premium, pay copays at visits, and still need to meet their yearly deductible which can vary based on plan type. Those that do not receive any of the above may purchase insurance through the marketplace or pay out of pocket. The U.S. territories follow similar health insurance practices.
Puerto Rico became a U.S. territory in 1898 when the island was ceded to the United States by Spain. In 1917, U.S. citizenship was granted to Puerto Ricans born after April 25th, 1898 (Foreign Relations of the United States, 1952–1954, United Nations Affairs, Volume III – Office of the Historian, 1952.). Puerto Rico is an island located between the Caribbean Sea and the North Atlantic Ocean. The island is 1,150 miles (1,851 km) from the east coast of the United States and has an area of approximately 3,515 square miles (U.S. Census, 2021). There is a population size of about 3.3 million people.
Puerto Rico receives less federal funding for healthcare than any of the 50 states. More than half of the people on the island depend on Medicare, Medicare Advantage, or Medicaid. The medical reimbursement rate for Medicare in Puerto Rico is 70% less than any state. (Roman, 2015). Out of all of the U.S. territories, Puerto Rico is the only one that the American Care Act applies to. In total, there are 66 hospitals on the island, 52 private and 13 public, and one federal (Dennis, 2020). Puerto Rico is poorer than the poorest U.S. states leading to several issues within its healthcare system. Hospitals have been known for closing wings, laying off employees, and limiting services due to funding. Patients also face long wait times to see a medical professional, sometimes waiting up to 13 hours before being seen at the emergency department and six to eight months to see a specialist (Begnaud, 2022).
In 1898, Spain also ceded Guam to the United State under the jurisdiction of the U.S. Navy. In 1950, U.S. citizenship was granted to all people living in Guam at that time, and the island was officially declared a U.S. territory. At this time, federal jurisdiction was also transferred from the U.S. Navy to the United States. Guam is an island with an area of about 225 square miles located in Micronesia (U.S. Department of Interior, 2004) approximately 5,986 miles (9,634 km) away from the west coast of the United States. They have a population size of 159,358.
The U.S. Department of Health and Human Services declared Guam as a Health Professional Shortage Area as well as a Medically Underserved Area (2020). Guam has only two civilian hospitals and one hospital for the U.S. Navy and their dependents. The island has more than 300 licensed physicians, 28 dentists, 6 counselors, and 11 optical centers (Guam | PIHOA, n.d.). There is a need for Primary care physicians, mental healthcare, and dental care on the island. For patients with more sophisticated procedures and treatment needs they may have to travel to Hawaii to receive more advanced care (Say & Thomson, 2003). One way the United States tries to assist Guam with its shortage is by offering debt relief to stateside doctors to work in Guam for a duration of time (Carlos, 2022). Medicaid and Medicare are available on the island as well as private insurance. Guam is the only U.S. territory that provides all mandatory Medicaid benefits as well as many optional benefits. Coverage is based on income eligibility referring to a local poverty guideline of up to 133% of the Guam poverty level (U.S. Department of Health and Human Services, 2020).
The U.S. Virgin Islands were bought from Denmark in 1917 by the United States. In 1927, the people of the islands were granted U.S. citizenship. The U.S. Virgin Islands are a string of about 50 islands, only four of which are inhabited, located 1,236 miles from the east coast of the United States. USVI has an area of approximately 133 square miles. Their population size is 87,416.
The U.S. Virgin Islands have two main full-service hospitals as well as several clinics and specialty healthcare centers. The hospital does provide emergency care which includes advanced cardiac treatment. For more serious issues, patients are airlifted to hospitals in either Puerto Rico or the mainland United States (Jula, 2018). The healthcare system in USVI has been challenged in recent years due to an intense hurricane in 2017 that physically destroyed the hospitals and healthcare systems on the islands. In 2022, they are still replacing several buildings to withstand future hurricanes and using temporary buildings until construction is complete (FEMA, 2022). They follow similar insurance practices as the United States.
In 1900, the island of Tutuila was ceded to the United States. In 1904, Manu Island joined, and in 1925, an act of congress led to Swain Island joining. All these individual islands make up part of American Samoa. Similarly, to Guam, American Samoa was under the jurisdiction of the U.S. Navy until 1951. In 1967, American Samoa created its own constitution. Unlike other U.S. territories, the people of American Samoa have not been granted access to U.S. citizenship but are considered U.S. nationals (U.S. Department of the Interior, 2021). American Samoa consists of seven islands in the South Pacific approximately 4,847 miles (7,800km) away from the west coast of the United States. The total area of the islands is about 77 square miles. There is a population size of 55,100.
In American Samoa, all citizens have Medicaid. Healthcare is subsidized and patients will have a small copay for services. There is only one hospital and one pharmacy for all the islands. There is also a federally funded community health center and 5 satellite health clinics. There is no health insurance program except for the military and a few private companies. Most citizens pay out of pocket for healthcare (American Samoa | PIHOA, n.d.). Most physicians on the island are general practitioners and lack exposure to specialty care. Sometimes, clinics may not even have a practitioner due to the shortage of physicians, nurses, and other healthcare professionals. When specialty care is required, a patient may be referred to the mainland United States. The hospital provides air travel for those patients, but it has to be paid for by the family. When longer term specialty care is required, families may not return to American Samoa due to ongoing treatment (III.A.1. Program Overview – American Samoa – 2020).
The Northern Mariana Islands became a U.S. territory in 1947 when the Treaty of Versailles was signed by Japan. Once this was in place, people of CNMI became U.S. citizens. CNMI consists of 14 islands within the Pacific Ocean located approximately 5,871 miles (9,448km) away from the west coast of the United States. The total area of the islands are approximately 184 square miles. Their population size is 53,883.
CNMI has one hospital, one medical laboratory, 3 community health centers, 5 private health clinics, and a community guidance center for mental health and substance abuse for all of the islands. The islands have a total of 31 physicians, 3 dentists, 4 pharmacists, and 123 nurses for a population of almost 60,000 (CNMI | PIHOA, n.d.). CNMI has a 100% fee-for-service delivery system (Northern Mariana Islands | Medicaid, n.d.).
One major social determinant of health that affects the U.S. Territories are their geographic location and what this means for their relationship to the United States and to other resources. These territories are various-sized islands, some right off the coast and some in the middle of the open sea. By being in remote locations away from the mainland United States, they face delays in obtaining testing equipment and delays in sending samples to necessary labs for testing if inaccessible on the island. The impacts of these delays are exacerbated during pandemic. The location of the territories also makes them more prone to experience detrimental natural disasters that cause immense damage with already limited resources which was seen during the 2009 influenza pandemic. Natural disasters such as hurricanes and typhoons exacerbate already fragile healthcare systems and infrastructure within the U.S. territories.
Natural disasters occur within the United States, but the impacts are incomparable to the U.S. territories in terms of deaths, damaged infrastructure, access to support and funding, and economic impact. The U.S territories have taken several strikes from multiple hurricanes and typhoons within the past five years, pre pandemic and during the pandemic. In 2018, there was Category 5 Super Typhoon Yutu, which was the largest storm worldwide since 1935. This storm affected both Guam and CNMI. Communities were destroyed by wind speeds above 180 miles per hour and about 10.5 inches of rainfall per hour (Chiu et al., 2021). This storm took a drastic toll on the public health infrastructure of these two territories. As of October 2020, just months before the COVID-19 pandemic was declared, only 30% of the homes destroyed during the 2018 typhoon were repaired in CNMI (Limtiaco, 2021). There were also delays in federal funding that were necessary to fix roads, schools, and public infrastructure with over year-long wait times for FEMA approval.
In 2017, Hurricane Irma and Hurricane Maria hit Puerto Rico and USVI within two weeks of one another causing widespread power outages and water service interruptions for several days weakening their physical infrastructure. Puerto Rico’s entire power grid was inoperable, over 95% of the population lacked access to drinking water, and 28% of federally qualified health centers were damaged (Romo, 2022). USVI faced almost an entire territory-wide blackout. Puerto Rico did experience a territory- wide blackout which is considered the longest blackout in U.S. history (Schwind, 2020). It took 11 months to restore all of Puerto Rico’s electricity. During this time, healthcare teams were unable to keep up with the demand (Acevedo, 2020). There have been consistent power outages in Puerto Rico since Hurricane Maria’s damage. In Puerto Rico, prolonged power outages and a lack of disaster management planning played a role in the death of 3,052 individuals who experienced extended disruptions to medical care (Rodriguez-Madera et al, 2021). The long-term effects of these natural disasters are still playing a role in how COVID-19 is affecting these territories. This has affected the current situation in 2022 because these areas were never able to fully rebuild and gain their normalcy before the pandemic began. Essentially, they were kicked down before they could ever get back up.
These disasters have also put stress on Medicaid funding, which is capped within the U.S. territories (U.S. Congress. United States Code: Social Security Act, 42 U.S.C. §§ 301- Suppl. 4 1934). Hurricanes increase the demand for Medicaid, but the damage that ensued from hurricanes makes it difficult for the U.S. territories to meet state matching requirements necessary to receive more Medicaid funds. This has also led to decreases in tourism which bring in a large amount of economic revenue for territories already facing year-long recessions and lead to more health care providers leaving the territories.
The goal of this thesis is to provide a descriptive analysis that compares and contrasts COVID-19 vaccination rates and mortality rates in the United States and each U.S. territory while reviewing social and cultural contexts that may relate to these trends as well as to the effectiveness of the methods used by the United States to support the U.S. territories throughout the pandemic. Sources of information and data for this project include targeted reviews of literature and of publicly available data on the COVID-19 pandemic.
Peer-reviewed research articles were systematically found through the use of PubMed, Google Scholar, and the Harvard University Global Health Education and Learning Incubator. Sources sought out included information regarding previous infectious disease outbreaks within the U.S. territories, discussion of health disparities related to race and racism and other social factors, and information regarding the COVID-19 pandemic. U.S. Territories’ government websites allowed for exploration of policies put in place during the COVID-19 pandemic. Encyclopedia Britannica served as a source providing historical information regarding healthcare and government information for each territory. This information is primarily developed in the literature review sections above.
A descriptive analysis was conducted of publicly available COVID-19 health data from the World Health Organization and the territories’ government websites. The dependent variables examined included mortality rates (deaths from COVID-19 per 100,000 people) and vaccination rates. Vaccination rates are divided into 3 categories as defined by the WHO:
- One dose – having had one dose of a two-dose mRNA vaccination series (Moderna and Pfizer)
- Two doses – considered “fully vaccinated”, having had two doses or a completed vaccination series or one dose of a single dose vaccination (Johnson and Johnson)
- Boosted – being fully vaccinated and receiving one additional COVID-19 vaccine after August 13, 2022
Although no causal analyses were completed during this project, conceptually the key independent variables considered are location (specific U.S. Territories) and aspects of the territories’ social and cultural contexts that may have impacted the outcomes of the pandemic and the efficacy of public health measures. Below, descriptive COVID-19 data and analyses of these data are provided to allow for descriptive comparisons and contrasts between the United States and its territories.
| Location | Deaths per 100,000 people |
|---|---|
| American Samoa | 56.16 |
| Guam | 221.00 |
| Northern Mariana Islands | 60.81 |
| Puerto Rico | 161.98 |
| U.S. Virgin Islands | 113.96 |
| United States | 305.46 |
Table 1: Mortality Rates
The data illustrated in Table 1 are the mortality rates, deaths per 100,000 people, from COVID-19 for the United States and the U.S. territories. Even though the population sizes of each location are drastically different, the mortality rate provides us with a standard making this data comparable. This data was sourced from the WHO Coronavirus Dashboard on September 25, 2022. Data collection for mortality rates began on January 3, 2020. These rates reflect the time period of January 3, 2020, to September 23, 2022.
| One Dose | Two Dose | Booster | |
|---|---|---|---|
| American Samoa | 81.32% | 75.05% | 43.77% |
| Guam | 91.97% | 83.55% | 42.74% |
| Northern Mariana Islands | 77.86% | 76.35% | 40.46% |
| Puerto Rico | 100% | 94.73% | 58.21% |
| U.S. Virgin Islands | 66.04% | 53.70% | Unknown |
| United States | 81.08% | 67.05% | 32.47% |
Table 2: Vaccination Rates
The data in Table 2 demonstrate vaccination rates. All of these rates were collected on September 25, 2022 and were at the time the most up-to-date data. All data shown except for the USVI was collected from the WHO Coronavirus Dashboard and reflects collection from the dates January 3, 2020, to September 23, 2022. The data for USVI was unavailable on the WHO dashboard. It was collected on September 25, 2022, from the Virgin Islands Department of Health’s COVID-19 Dashboard. This information was last updated on May 25, 2022.
The United States has the highest mortality rate for COVID-19, as seen in Table 1. The U.S. territory with the highest mortality rate for COVID-19 is Guam. Guam did fare better than the United States for mortality rates, but still ranks second highest overall.
Puerto Rico and the U.S. Virgin Islands are in the middle with Puerto Rico having the third highest mortality rate following Guam and the USVI with the fourth highest. Following Puerto Rico was the CNMI. American Samoa had the lowest mortality rate. The mortality rate of the United States is almost double that of Puerto Rico, about 3 times the mortality rate of the USVI, and almost 5 times the rate of American Samoa and the CNMI.
CNMI and American Samoa have very similar mortality rates for COVID-19 as reflected in Table 1. Of all the U.S. territories, Guam has the highest mortality rates from COVID-19. Guam’s mortality rate is almost double that of the USVI, and approximately 4 times that of American Samoa and the CNMI. Puerto Rico had the second highest mortality rate of the U.S. territories at about ¾ the rate of Guam. Puerto Rico has about 3 times the mortality rate of American Samoa and the CNMI. Interestingly enough, Puerto Rico and the USVI have a smaller difference in mortality rates than Puerto Rico and Guam. USVI has the third highest mortality rate of the U.S. territories following Puerto Rico. The USVI has about double the mortality rate of American Samoa and the CNMI.
Puerto Rico is leading with vaccination rates regardless of how many doses, with 100% of the population reported. For the first dose, USVI has the lowest rates (66.04%) followed by CNMI (77.86%). USVI has the lowest vaccination rates overall; however, the data is incomplete and has not been updated as frequently as the other locations.
Guam has the second highest rate of vaccination for dose one (91.97%). American Samoa has the third highest rate for one dose (81.32%) which is closely followed by the United States (81.08%). The United States is second last for the second dose of vaccination and last for the booster. Guam has the second highest second dose rates followed by CNMI and then American Samoa. American Samoa is the second highest for booster rates followed by Guam and CNMI.
When compared to vaccination rates across the Territories, the vaccination rates in the United States sat in the middle for the first dose, second to last for the second dose, and last for the booster. The CNMI had lower vaccination rates for the first dose compared to the United States by about 3% but fared better for dose two and the booster by about 8%. The USVI has lower rates than the United States for all vaccination rates.
American Samoa had about the same vaccination rates for dose one compared to the United States but fared better for dose two by about 8% and the booster by about 10%. Guam and Puerto Rico both fared better across all vaccination rates compared to the United States by over 10% for each.
Puerto Rico excelled in vaccination rates, possibly fully vaccinating its population with at least one dose. They also excelled overall in vaccinating most of the population with two doses and over half with the booster. Guam also had fairly high vaccination rates following Puerto Rico. Although the CNMI had the second lowest vaccination for the first dose of the U.S. territories, they were on par with Guam for the second dose.
Guam, American Samoa, and the CNMI all had similar booster rates at about 40%. The USVI fell short for vaccination rates, although the data was limited.
This research examines mortality rates and vaccination rates and explores social and communal contexts to compare and contrast the impacts of the COVID-19 pandemic in the United States and the U.S. territories. This is a descriptive study in which the goal is not to establish causality; instead, the goal is to contextualize the information derived from various sources regarding the outcomes of the COVID-19 pandemic while also examining key disparities in order to point to additional research questions. These contextual connections are not causal. There is also room for further exploration of specific contextual issues – e.g., health care, environment, and other social conditions – that were discussed throughout the literature review. Although these claims are not causal, this descriptive study is setting the groundwork for new, meaningful questions to be brought forth regarding the U.S. territories and their outcomes from this COVID-19 pandemic.
As previously mentioned, the CNMI and American Samoa have similarly low mortality rates, the lowest among all locations studied in this project. They are both extremely isolated in the Pacific Ocean which may have been beneficial looking at mortality rates. They also have similarly small population sizes. These two territories did not see COVID-19 cases until over a year into the pandemic, which suggests geographic contexts may have been contributing advantages to keeping COVID-19 out. In addition, CNMI and American Samoa did not see communal spread until months after their initial cases, likely due to their exhaustive public health practices to mitigate spread. Since these territories are in the USAPI, they followed similar practices such as heightened surveillance, testing requirements, contact tracing, and multiple tests during quarantine.
Guam is also a member of the USAPI and followed similar precautions. When Guam had its first case of COVID-19, the entire island practically shut down which is why it is surprising why Guam’s mortality outcomes were so vastly different from the CNMI and American Samoa. Guam had the highest mortality rate of the U.S. territories. Although this analysis cannot explain why this is, there are contextual findings that stand out when looking at Guam’s health outcomes from the COVID-19 pandemic. Guam was declared as a Health Professional Shortage Area and Medically Underserved area in 2020 by the Department of Health and Human Services. This deserves further exploration, as limited health professionals may have contributed to the COVID-19 outcomes in Guam. Throughout the pandemic there were many limitations including lack of staff in Guam that seems to support the Department of Health and Human Service claims. This points to questions regarding whether staffing issues are contributing to the population being underserved regarding health care. Research questions moving forward could aim to address whether Guam’s health professional shortage limits their ability to combat infectious diseases, including in this particular case, the COVID-19 pandemic.
In addition, a unique event regarding the USS Theodore Roosevelt may have had its own health implications for Guam. There was limited information regarding how the USS Theodore Roosevelt impacted COVID-19 outcomes within the territory. What is known about the situation with the USS Theodore Roosevelt is that over 1,000 sailors who had tested positive for COVID-19 were quarantined in Guam in hotels. The community was not supportive of these actions, as it put the people of Guam at an unfair risk. There is information out there regarding the political implications of the entire situation and how to better handle similar situations moving forward; however, there is a lack of information regarding the health implications of the incident. This poses the question of whether the USS Theodore Roosevelt contributed to the spread of COVID-19 in Guam. This seems like a very important piece of information when discussing the spread of COVID-19 in Guam. There is little publicized about this major event after 2020. Whether or not this military aircraft carrier contributed to spread of disease is unknown and should be explored in the future, especially because Guam’s mortality rates were relatively much larger than the rest of the U.S. territories. This could have implications for military and public health policy and practices.
Geographic location was discussed above as creating potential limitations to combat disease due to the lack of lab facilities for testing in some territories, shipping tests and vaccinations, etc., due to relative geographic isolation. However, what was not explored was ways in which geographic location might be a potential factor in actually limiting the spread of COVID-19. As discussed earlier, the CNMI and American Samoa were some of the farthest islands from the U.S. mainland as well as any other mainland. As reflected in the data, they had the lowest mortality rates. Puerto Rico and the USVI are the closest islands to the U.S. mainland. As seen in the discussion above, Puerto Rico still had tourists visiting the island from the United States throughout the current pandemic, possibly due to how close it is: could it be that Puerto Rico was and is a destination vacation for those who are bored of a pandemic but faced more restrictions on international travel? Puerto Rico had the second-highest mortality rate of the U.S. territories, and the USVI followed behind those rates. Future research could explore how travel rates and travel restrictions may have impacted the outcomes of the COVID-19 pandemic in the US Territories. Seeing if limiting tourism from the United States, which was considered domestic travel, limited the spread of COVID-19 could be important to mitigating the spread of diseases in the future.
Puerto Rico claimed great success in getting their population vaccinated as seen in Table 2. One major reason for this success seems to be community-based efforts with a high degree of collaboration. For example, vaccinations and masks were not politicized as they had been within the United States (Espada M., 2021). Once vaccines were available, healthcare professionals got vaccinated quickly to create trust for the vaccine and prioritized getting vaccines to rural communities. Puerto Rico also had an interesting tactic of distributing vaccinations and went as far as holding vaccination events at beaches and bars, which ultimately seems like it paid off in the end. Public and private health sectors worked together for a common goal in Puerto Rico, which was to mitigate spread and promote safety during the COVID-19 pandemic. Other U.S. territories also showed common themes of community-based approach that focused on coming together and fighting against COVID-19. This allowed the territories to outshine the United States in regard to vaccination rates and fare better in terms of mortality rates. The USAPI had support for Guam, the CNMI, and American Samoa through efforts to mitigate spread such as restricting travel, enhanced testing requirements for those in quarantine, and enhancing surveillance for these territories. Future research might explore whether the size and unity within the communities in the U.S. territories contribute to their relatively more successful public health outcomes compared to the outcomes seen in the United States.
There were other themes seen across all U.S. territories during the COVID-19 pandemic that may have affected health outcomes. One of these themes was the lack of healthcare staff which seems like a consistent issue that preceded the current pandemic. The United States gives better opportunities, funding, and provides better training for doctors compared to the U.S territories, so many doctors within the territories leave for opportunities in the United States. This leaves the territories vulnerable as they do not have the necessary providers to provide care for everyone effectively on the islands. This was an issue during the COVID-19 pandemic. The United States also struggled with staffing, however, more resources were readily available such as the military and the National Guard. The Military and National Guard were also deployed for short periods of time within the U.S. territories to help distribute vaccinations, but staff support in healthcare facilities and for testing was still limited.
There were also themes of ineffective or damaged public health infrastructure in some territories that were noteworthy in the background research. In Puerto Rico, early in the pandemic there were inconsistencies with leadership that affected how the COVID-19 pandemic was being portrayed to the public and did not give Puerto Rico the consistent support that was needed for a pandemic. Puerto Rico and the USVI were still dealing with long term damage from major hurricanes when the COVID-19 pandemic began, including persistent power outages and rebuilding USVI’s main hospital. The U.S. territories lacked sufficient time to rebuild public health infrastructure prior to the COVID-19 pandemic which probably played a role in the outcomes. Without a solid foundation for public health and healthcare, these territories were ill-prepared to combat a new large-scale infectious disease.
It was seen during the 2009 influenza pandemic that funding was an issue that affected effectiveness of public health responses. Several U.S. territories actually acknowledged that the funding from the United States provided during the COVID-19 pandemic was a step in the right direction for the U.S. territories to combat COVID-19. The funding allowed the U.S. territories to open vaccination clinics, fix public health infrastructure, and expand laboratories. This was also the first time that Puerto Rico received equal healthcare funding from the United States through the Coronavirus Relief Fund (CARES Act). Future research should explore the specific ways that access to funding, funding amounts, and timing may have impacted the outcomes of the COVID- 19 pandemic in the U.S. territories.
Although this project had initial goals of exploring social and cultural conditions including how race and ethnicity played a role in health outcomes for the COVID-19 pandemic in the US territories, race and ethnicity was quite complex and for many reasons not directly addressed in this project. an Although extensive searches were conducted for COVID-19 outcome data that is disaggregated by race and ethnicity in the US territories, these data were lacking: there were no clear, standardized sources for this kind of publicly available data found during the period of research. Several new questions did emerge however while conducting this research, including questions about the prominence of predominant U.S. racial and ethnic categorization to the distinct cultural and political contexts of the U.S. territories. In the future, I would like to explore further why race is not accounted for within the U.S. territories when it comes to looking at vaccination rates and mortality rates as it is within the United States. Racial and ethnic identity do differ among these populations, and I strongly believe it is worth exploring in order to get a better understanding of the cultural influences in the U.S. territories data collection methodology and in health disparities faced by the territories.
This research has its limitations. One limitation was that at the time of writing this thesis, the COVID-19 pandemic is still in fact a pandemic. This is an ongoing and changing disease with worldwide impacts that is being hypothesized to be around long term. In the past three years, we have already seen several variants of COVID-19. Since this is an ongoing disease, all points of discussion in this thesis are about ongoing social impacts and not about static outcomes. Another limitation of this study was the lack of centralized and updated public data available for COVID-19, especially for the U.S. territories. Finding data was challenging, and several databases were searched throughout this process. The CDC lacks information about the U.S. territories. Originally, government health sites were used for data; however, data collection was different per each U.S. territory as far as when data was being updated, how data was being collected, and how data was being portrayed. The World Health Organization COVID-19 Dashboard was utilized later during the project. The WHO dashboard is the most reliable source, but still faces its own limitations, as data is reported by country or territory. Since Puerto Rico is larger, data was easier to find and more accessible. For other territories, particularly American Samoa, data was challenging to find or overall extremely limited. Data collection is also ongoing and may look different in a few years or even a few months. Since beginning this project, there have already been changes in data trends.
There are also different timelines for the United States and each U.S. territory as they all were affected by COVID-19 at different times, some as early as January 2020, and some as late as April, 2022. With these limitations also come strengths as this work contributes to the works of public health.
Despite the limitations of this study, there are several contributions to public health literature. This research contributes to public health research regarding health disparities in the U.S. territories which is lacking, especially surrounding the COVID-19 pandemic. Although these claims are not causal, exploring social contexts are vital in attempting to understand the layers that contribute to understanding the public health outcomes in the U.S. territories. It is important to tell the stories that are oftentimes overlooked, in this case, the COVID-19 health outcomes in the U.S. territories. This research also allows us to think about ways to examine health disparities in the U.S. territories in the future. Potential case studies can be done moving forward to potentially pinpoint reasons why the U.S. territories were relatively successful in their health outcomes during the COVID-19 pandemic. This study also brought forth different social, environmental, and policy contexts that opens the door for further exploration.
This project aimed to examine the vaccination rates and mortality of the COVID- 19 pandemic while discussing the social and cultural conditions of the U.S. territories in order to compare and contrast those outcomes with the United States. Although this project did not offer explanations as to why these differences in health outcomes occurred during the COVID-19 pandemic, it created a valuable foundation to begin exploring new potential topics as was mentioned in the discussion. In doing so, it was seen that there are notable differences in the measured outcomes of vaccination rates and mortality rates which bear on population health and public health. The U.S. territories overall seemed to fare better than the United States with both variables except for the U.S. Virgin Islands’ vaccination rates. There are lessons to be learned from the COVID-19 pandemic pertaining health policy and implementation as well as travel restrictions and staffing. All of these factors contributed in one way or another, and these factors should be further explored in more depth to see to what extent their role played in these health outcomes.
By examining these factors in the future in more depth, we can make conclusions about what works better and what does not work when trying to mitigate the spread of disease.
I would like to express my gratitude to my amazing mentors who have helped guide me during this project. Dr. Robin Shura and Dr. Jennifer King have shown immense support throughout this process, and I am so thankful for that. I also would like to thank Dr. Derek Kingsley who opened the doors for my research experience teaching me the foundations of research that I have since been able to build upon. I would also like to thank the McNair Scholars Program at Kent State who helped me realize my true potential. Thank you to the Honors College as well for pushing me to even write a thesis. To my academic advisor, Kristofer Braxton, I am also extremely grateful for pushing me to be not just a great student, but a better person. Lastly, I want to thank my partner who has been very supportive of this work and has heard me go on and on about this topic for a year and a half. I am so appreciative for all the support.
- Acevedo, N. (2020, September 20). On Hurricane Maria’s third anniversary, Puerto Rico sees more pain and little progress. NBCNews.com. Retrieved September 26, 2022.
- American Samoa | PIHOA: (n.d.). Retrieved October 8, 2022, from https://www.pihoa.org/american-samoa/
- American Samoa. U.S. Department of the Interior. (2021, February 19). Retrieved June 28, 2022.
- Begnaud, D. (2022, September 21). Health Care System “collapse”: Doctors, experts sound alarm over Puerto Rico’s medical system. CBS News. Retrieved October 8, 2022, from https://www.cbsnews.com/news/puerto-rico-health-care-system- collapse/
- Benefits. Medicaid. (n.d.). Retrieved October 26, 2022, from https://www.medicaid.gov/medicaid/benefits/index.html
- Bureau, U. S. C. (2021, October 28). Census Bureau releases 2020 Census population and Housing Unit counts for the U.S. Virgin Islands. Census.gov. Retrieved August 8, 2022.
- Bureau, U. S. C. (2021, December 16). 2010 Island Areas – Commonwealth of the Northern Mariana Islands dataset. Census.gov. Retrieved August 6, 2022.
- Bureau, U. S. C. (2022, July 11). 2020 island areas censuses: American samoa. Census.gov. Retrieved August 8, 2022.
- Bureau, U. S. C. (2022, July 11). 2020 island areas censuses: Commonwealth of the Northern Mariana Islands (CNMI). Census.gov. Retrieved August 8, 2022.
- Bureau, U. S. C. (2022, July 11). 2020 island areas censuses: Guam. Census.gov. Retrieved August 8, 2022.
- Carlos, D. R. (2022, September 16). Letter: Dire need of physicians now, future. guampdn.com. Retrieved October 8, 2022, from https://www.guampdn.com/opinion/letter-dire-need-of-physicians-now-future/article_c4fd9c30-34ed-11ed-893e-b7a5d71cf0dc.html
- Centers for Disease Control and Prevention. (2018, June 26). Seasonal flu vs. pandemic flu infographic. Centers for Disease Control and Prevention. Retrieved July 9, 2022.
- Centers for Disease Control and Prevention. (2020, November 24). Health Disparities.Centers for Disease Control and Prevention. Retrieved June 28, 2022.
- Centers for Disease Control and Prevention. (2021, July 14). How coronavirus spreads. Centers for Disease Control and Prevention. Retrieved June 28, 2022.
- Centers for Disease Control and Prevention. (2021, September 30). Social Determinants of Health. Centers for Disease Control and Prevention. Retrieved June 28, 2022.
- Centers for Disease Control and Prevention. (2021, November 2). Types of influenza viruses. Centers for Disease Control and Prevention. Retrieved July 9, 2022.
- Centers for Disease Control and Prevention. (2022, January 5). CDC Museum Covid-19 Timeline. Centers for Disease Control and Prevention. Retrieved June 28, 2022.
- Chiu, A., Mooney, C., & Eilperin, J. (2021, July 15). Extreme category 5 typhoon, the worst U.S. storm since 1935, leaves Northern Mariana Islands devastated. The Washington Post. Retrieved October 8, 2022, from https://www.washingtonpost.com/energy-environment/2018/10/24/extreme-category-typhoon-yutu-makes-devastating-landfall-northern-mariana-islands-us- commonwealth/
- CNMI | PIHOA: (n.d.). Retrieved September 23, 2022, from https://www.pihoa.org/cnmi/
- Coto, D., “Missteps mar Puerto Rico’s response to coronavirus,” AP News (April 2020), https://apnews.com/article/e5ba6c2639ee52dad5e367d2228ac764
- Dennis, A. (2020, April 9). Covid-19 and the collapse of Private Hospitals in Puerto Rico. COVID-19 and the Collapse of Private Hospitals in Puerto Rico – Eyes on the Ties. Retrieved October 8, 2022, from https://news.littlesis.org/2020/04/09/covid-19-and-the-collapse-of-private- hospitals-in-puerto- rico/#:~:text=According%20to%20the%20Health%20Services,public%2C%20an d%20one%20is%20federal.
- Dopson, S. A. (2016). Improving the Public Health Infrastructure Capacity in the U.S. Pacific Territories. Journal of Health Care for the Poor and Underserved, 27(4), 1632–1637.
- Espada, M. (2021, November 2). How Puerto Rico depoliticized the COVID-19 vaccine. Time. Retrieved October 22, 2022, from https://time.com/6113069/puerto-rico- vaccination-rate-covid-19/
- Feldscher, K. (2021, August 11). What will it be like when covid-19 becomes endemic?News. Retrieved October 22, 2022, from https://www.hsph.harvard.edu/news/features/what-will-it-be-like-when-covid-19- becomes-endemic/
- Firozi, P., & Shammas, B. (2021, September 20). American Samoa, one of the last places without coronavirus, has first infection. The Washington Post. Retrieved October 10, 2022, from https://www.washingtonpost.com/health/2021/09/19/american- samoa-first-covid-case/
- Foreign Relations of the United States, 1952–1954, United Nations Affairs, Volume III – Office of the Historian. (October 9, 1952). Retrieved June 27, 2022.
- Guam | PIHOA: (n.d.). Retrieved October 8, 2022, from https://www.pihoa.org/guam/
- Home: Virgin islands department of health. Home | Virgin Islands Department of Health. (2022, September 22). Retrieved September 25, 2022, from https://www.covid19usvi.com/
- Joint Region Marianas Public Affairs. (2021, April 5). US Army Medical Professionals administer COVID-19 vaccines in Saipan. U.S. Indo-Pacific Command. Retrieved October 8, 2022, from https://www.pacom.mil/Media/News/News-Article- View/Article/2561696/us-army-medical-professionals-administer-covid-19- vaccines-in-saipan/
- Jula, M. (2018, June 3). Hurricanes drove more than 1,000 medical evacuees from the Virgin Islands. many can’t go home. Grist. Retrieved October 15, 2022, from https://grist.org/article/hurricanes-drove-more-than-1000-medical-evacuees-from- the-virgin-islands-many-cant-go-home/
- Limtiaco, S. (2021, February 4). Many CNMI homes still not repaired from 2018 typhoon. guampdn.com. Retrieved August 30, 2022, from https://www.guampdn.com/news/local/many-cnmi-homes-still-not-repaired-from- 2018-typhoon/article_7b4c89d2-c43a-5ac2-86cd-41d168d7fff5.html
- Link, B. G., & Phelan, J. (1995). Social Conditions As Fundamental Causes of Disease. Journal of Health and Social Behavior, 80–94.
- Mackey, K., Ayers, C. K., Kondo, K. K., Saha, S., Advani, S. M., Young, S., Spencer, H., Rusek, M., Anderson, J., Veazie, S., Smith, M., & Kansagara, D. (2021). Racial and Ethnic Disparities in COVID-19–Related Infections, Hospitalizations, and Deaths.
- Mazzei, P. (2020, April 21). Puerto Rico Lags Behind Everywhere Else in U.S. in Virus Testing. The New York Times.
- Northern mariana islands. Medicaid. (n.d.). Retrieved September 23, 2022, from https://www.medicaid.gov/state-overviews/cnmi.html
- Ollove, M. (2022, March 25). Health worker shortage forces states to Scramble. The Pew Charitable Trusts. Retrieved October 8, 2022, from https://www.pewtrusts.org/en/research-and- analysis/blogs/stateline/2022/03/25/health-
- Patron, M. (2017, April 8). The exodus of Puerto Rico’s doctors has strained its health care system. NBC News. Retrieved May 11, 2022.
- Richardson, M. (2021, January 14). American Samoa closed its borders in March. stranded residents are finally going home. https://www.hawaiinewsnow.com. Retrieved October 10, 2022, from https://www.hawaiinewsnow.com/2021/01/15/first-american-samoan-repatriation- flight-set-january-honolulu/
- Rodríguez-Madera SL, Varas-Díaz N, Padilla M, Grove K, Rivera-Bustelo K, Ramos J, Contreras-Ramirez V, Rivera-Rodríguez S, Vargas-Molina R, Santini J. (2021, Nov 10). The impact of Hurricane Maria on Puerto Rico’s health system: post-disaster perceptions and experiences of health care providers and administrators. Glob Health Res Policy. 6(1):44. doi: 10.1186/s41256-021-00228-w. PMID: 34753513; PMCID: PMC8577961.
- Rodríguez Velázquez , V., & Colón Almena, V. s. (2020, April 14). Passengers arrive in Puerto Rico from areas of greatest contagion by coronavirus in the US. Centro de Periodismo Investigativo. Retrieved September 25, 2022, from https://periodismoinvestigativo.com/2020/04/passengers-arrive-in-puerto-rico- from-areas-of-greatest-contagion-by-coronavirus-in-the-us/
- Roman, J. (2015). The Puerto Rico Healthcare Crisis. Annals of the American Thoracic Society, 12(12), 1760–1763.
- Romo, V. (2022, September 20). Puerto Rico has lost more than power. The vast majority of people have no clean water. NPR. https://www.npr.org/2022/09/20/1123984002/hurricane-fiona-puerto-rico-lost- more-than-power-vast-majority-no-clean-water
- Say, R. E., & Thomson, R. (2003, September 6). The importance of patient preferences in treatment decisions–challenges for doctors. BMJ (Clinical research ed.). Retrieved October 8, 2022, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC192849/
- Schwind, K. (2020, May 26). What we can learn from the worst power outage in U.S. history. National Standby Repair. Retrieved September 4, 2022, from https://www.nationalstandby.com/blog/what-we-can-learn-from-worst-power- outage-us- history/#:~:text=The%20largest%20blackout%20in%20U.S.,longest%20blackouti. %20in%20U.S.%20history.
- Serrano-Roman, A. (2020, March 27). PR Went Through 3 Health Secretaries This Month As COVID-19 Spread; Chief Epidemiologist Resigns. CT News Junkie.
- Steinhauer, J. (2021, January 14). Overwhelmed, more states turn to National Guard for vaccine help. The New York Times. Retrieved September 19, 2022, from https://www.nytimes.com/2021/01/14/us/politics/coronavirus-vaccine-national- guard.html
- Stolyar, L., Orgera, K., & Rudowitz, R., 2021. (2021, May 18). Challenges in the U.S. Territories: COVID-19 and the Medicaid Financing Cliff. KFF. https://www.kff.org/coronavirus-covid-19/issue-brief/challenges-in-the-u-s- territories-covid-19
- The Associated Press. (2020, March 13). Puerto Rico announces its first confirmed coronavirus cases. ABC News. Retrieved September 25, 2022, from https://abcnews.go.com/Health/wireStory/puerto-rico-announces-confirmed- coronavirus-cases-69593953
- United States Code, 2012 Edition, Supplement 2, Title 48 – TERRITORIES AND INSULAR POSSESSIONS9-and-the-medicaid-financing-cliff/
- U.S. Congress. United States Code: Social Security Act, 42 U.S.C. §§ 301- Suppl. 4 1934
- U.S. Census Bureau quickfacts: Puerto Rico. (2021). Retrieved June 25, 2022, from https://www.census.gov/quickfacts/PR
- U.S. Census Bureau quickfacts: United States. (2021, July 1). Retrieved September 19, 2022, from https://www.census.gov/quickfacts/fact/table/US/PST045221
- U.S. Department of the Interior. (2004, February 14). War in the Pacific NHP: Archeology and history of guam (section A). National Parks Service. Retrieved July 10, 2022.
- U.S. virgin Islands Healthcare facilities advance toward recovery five years after the storms. FEMA.gov. (2022, September 30). Retrieved October 15, 2022, from https://www.fema.gov/press-release/20220929/us-virgin-islands-healthcare-facilities-advance-toward-recovery-five-years
- Weissman, M. A. (2021, April 29). U.S. Army Medical Team administers COVID-19 vaccines in Guam. Military Health System. Retrieved October 8, 2022, from https://health.mil/News/Articles/2021/04/29/US-Army-Medical-Team- Administers-COVID19-Vaccines-in-Guam#:~:text=A%20team%20of%20U.S.%20Army,Division%20at%20Army%20Garrison%20Hawaii.
- Welna, D. (2020, April 2). Guam locals unhappy with housing U.S. sailors from coronavirus-hit aircraft carrier. NPR. Retrieved October 10, 2022, from https://www.npr.org/sections/coronavirus-live- updates/2020/04/02/826262256/guam-locals-unhappy-with-housing-u-s-sailors- from-coronavirus-hit-aircraft-carri
- Westerman, A. (2022, March 18). Samoa locks down after recording its first community COVID-19 case. NPR. Retrieved September 25, 2022, from https://www.npr.org/2022/03/18/1087447176/samoa-locks-down-after-recording- its-first-community-covid-19-case
- World Health Organization. (n.d.). Who coronavirus (COVID-19) dashboard. World Health Organization. Retrieved September 25, 2022.
- Yang, L., Liu, S., Liu, J., Zhang, Z., Wan, X., Huang, B., Chen, Y., & Zhang, Y. (2020). Covid-19: Immunopathogenesis and Immunotherapeutics. Signal Transduction and Targeted Therapy, 5(1).
- III.A.1. Program Overview – American Samoa – 2020. American Samoa – 2020 – III.A.1. program overview. (n.d.). Retrieved July 10, 2022, from https://mchb.tvisdata.hrsa.gov/Narratives/ExecutiveSummary/be7a1b90-b6cb- 4716-ac6e-a27b897be87a.













