Article / Case Report
Consultant oncoradiologist, M.D, Radiological Department, Copenhagen University Hospital Herlev Gentofte, Denmark.
Gina Al-Farra,
Consultant oncoradiologist, M.D,
Radiological Department,
Copenhagen University Hospital Herlev Gentofte,
Denmark.
3 February 2024 ; 19 February 2024
Purpose: to visualize complication of antineoplastic /immunotherapy treatment.
Immunotherapy treatment can affect all organs and types of tissues, with manifestations that may appear acute or after prolonged treatment. Recognizing the side effects it is important, it may have a big impact in the treatment itself but also save the patient’s life, certain conditions can be life threatening (for example, pneumonitis). Immune checkpoint inhibitors (ICI) are widely used for the treatment of malignant neoplasms. Interstitial lung disease is a well-known immune-related adverse event, however, ICI-induced airway disease remains under-recognized [1].
Keywords: Immunotherapy, malignant melanoma, pneumonitis, immune-related adverse events (irAEs).
32- Years male patient treated with Ipilimumab for malignant melanoma, in complete remission. Three months after starting the treatment, complains about persistent cough and dyspnea. Secondary, annoying retrosternal pain and burning sensation, especially when breathing. The patient has no previews lung or airways disease.
Blood tests revealed elevated C-reactive protein levels, no eosinophilia. Border up levels of leucocytes. Spirometry with mild airflow obstruction.
The patient was referred to CT lungs on suspicion of pneumonitis.
Bronchoscopy performed after CT lungs, revealed edematous and erythematous tracheobronchial mucosa, and bronchial biopsy tissue exhibited marked inflammation and infiltration of CD8+ lymphocytes.
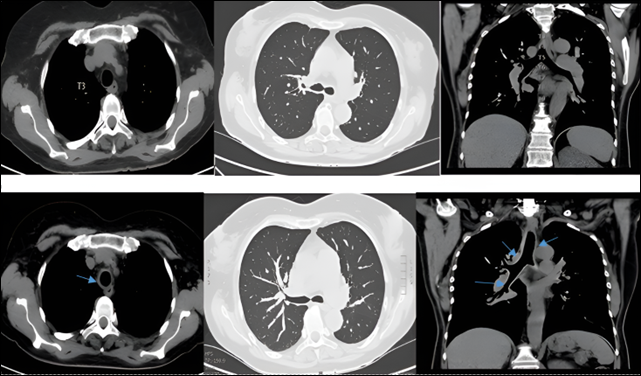 Unenhanced CT scan of lungs (with low dose), axial and coronal reconstruction, the upper row in the beginning of the treatment with Ipilimumab-normal findings. The lower row, three months after, shows thickened trachea and main bronchus bilaterally (blue arrows), but no lung changes.
Unenhanced CT scan of lungs (with low dose), axial and coronal reconstruction, the upper row in the beginning of the treatment with Ipilimumab-normal findings. The lower row, three months after, shows thickened trachea and main bronchus bilaterally (blue arrows), but no lung changes.
Computed tomography revealed diffuse thickening of the tracheobronchial walls and slights bronchiectasis predominantly in the lower lobes. No sign of pneumonitis or lung infection or activate of sarcoid.
Immune checkpoint inhibitors (ICI) are widely used for the treatment of malignant neoplasms. Interstitial lung disease is a well-known immune-related adverse event, however, ICI-induced airway disease remains under-recognized [1]. This is one case of Ipilimumab-induced tracheobronchitis presenting as persistent cough and dyspnea. Ceasing Ipilimumab, the inhaled corticosteroids, and long-acting beta-agonists gradually improved the symptoms, airflow obstruction, and radiographic findings.
Among the varied immune-related adverse events (irAEs), pneumonitis is well-known [2]; However, it is unknown whether chronic airway diseases such as chronic obstructive pulmonary disease (COPD) and asthma impact on the incidence of irAEs after ICI treatment [3].
This case suggest that pulmonary IRAEs secondary to ICIs may present as isolated bronchitis or bronchiolitis, with good outcomes following ICI withdrawal and systemic corticosteroids.
ICI-induced airway disease is a new pattern of immunotherapy induced lung toxicity, an under-recognized manifestation of immune-related adverse events.
Consent for image publication cannot be obtained as the case is more than 5 years old and the patient is deceased after severe relapse of melanoma.
- Kawakami N, Saito H, Takahashi S, Kajie S, Kato R, Shimaya K, Wakai Y, Saito K, & Sakashita M. Airway disorders associated with immune checkpoint inhibitor therapy: Two case reports and a systematic review. Semin Oncol. 2022 Dec;49(6):439-455. DOI: 10.1053/j.seminoncol.2023.01.003. Epub 2023 Feb 2. PMID: 36759235.
- Wassmer F, Suehs C, Boissin C, Bourdin A, & Charriot J. PD-L1 inhibitor-induced worsening of eosinophilic obstructive lung disease successfully rescued with anti-interleukin 5 receptor (IL-5R) therapy. J Allergy Clin Immunol Pract. 2021 Jan;9(1):567-569.DOI: 10.1016/j.jaip.2020.08.022. Epub 2020 Aug 22. PMID: 32841747.
- Wang H, Shi J, Wang X, Zhao H, Wang H. Acute exacerbation of asthma induced by combined therapy of programmed death-1 Blocker plus lenvatinib in a patient with advanced hepatocellular carcinoma. Eur J Cancer. 2021 Oct;156:122-124. DOI: 10.1016/j.ejca.2021.07.025. Epub 2021 Aug 21. PMID: 34428685.













