Article / Case Report
1University of kalamoon, Deir Atyiah, Damascus, Syria
2University of kalamoon, Deir Atyiah, Damascus, Syria
3Kalamoon University Hospital, Damascus, Syria
4Kalamoon University Hospital, Aleppo University Hospital, Damasacus, Syria
Adnan Ismail
Thoracic surgeon
Kalamoon University Hospital
Damascus
Syria
5 August 2020 ; 2 Septmber 2020
This report describes the case of a 39-year-old man with a mediastinal teratoma. For seven years the patient had been suffering a dyspnea on exertion. In the last few weeks, the dyspnea increased and new symptoms appeared such as dry cough, chest pain and palpitations. Computed tomography revealed a medium-sized tumor that was markedly compressing the superior vena cava and the right atrium. Surgery was performed, and a benign mature teratoma was diagnosed. Mature mediastinal teratomas are benign tumors, but they can be adherent to collateral structures in the chest leading to life threatening complications.
Key words: mediastinal tumor, teratoma, slow-growing.
Teratomas consist of all three primordial layers: ectoderm (skin and hair), mesoderm (bone, fat, and muscle), and endoderm (respiratory epithelium and gastrointestinal tract) [1]. They are categorized as either mature (benign) or immature (malignant) [3]. Additionally, benign teratomas can be either cystic (mostly benign) or solid (mostly malignant) or a combination of both [1]. This case focuses on mature cystic teratomas, commonly referred to as dermoid cysts.
Cystic teratomas occasionally occur in sequestered midline embryonic cell rests and can be mediastinal (7% of all teratomas). It has no sex predilection, but its current location correlates with age especially in adults during the third to fourth decade of life [2].
This rare benign neoplasia tends to be slow growing and many patients have no symptoms when the mass is discovered, often incidentally [1]. The present study describes the case of a patient who has gradually progressed symptoms related to the tumor size in the course of many years, and who later suffered from serious functional problems due to the tumor’s location and compression on the right atrium and the superior vena cava.
Benign teratomas of the mediastinum are rare, representing 8% of all tumors of this region [4]. Although they don’t have the metastatic potential, but malignant transformation occurred in 1-3% of mature cystic teratomas (MCTs), usually in postmenopausal women [5].
When forming a differential diagnosis for teratomas, we should think about neurogenic tumors (28% of mediastinal masses), thymomas, lymphomas, other germ cell tumors, pericardial cysts and other miscellaneous lesions [6].
In some cases, the mediastinal teratomas can be ruptured and present in a completely different scenario. The tumor can grow very fast and the symptoms progress within few months. Thus, the tumor is a life-threatening condition and urgent surgery must be performed [7].
In our case, the patient presented with the classic symptoms, radiological findings and histological appearance associated with mature teratoma. As soon as the teratoma is diagnosed, the surgeon must determine the operability of the tumor, whilst also weighing up the risks and benefits of surgery.
Some surgeons prefer the VATS technique, which is minimally invasive and requires shorter recovery period [8]. To the best of our knowledge, we think the open-surgery is the best choice for tumor resection despite their type or progression, because only the open-surgery provides us with the visual information required to completely resect the tumor and accurately diagnose the condition.
The tumor may be adherent to surrounding structures, necessitating resection of the pericardium, pleura, or lung. The present patient showed no adherence or invasion into local mediastinal structures, but the superior vena cava was markedly compressed.
When complete resection is achieved, it results in excellent long-term cure rates with little chance of recurrence and when complete resection is impossible, partial resection often leads to symptom relief, frequently without relapse.
In conclusion, mature mediastinal teratoma are usually benign, slow-growing tumors accompanying with insidious symptoms which make the condition neglected or misdiagnosed with other conditions. Therefore, we should warn our physicians and consider tumors as a differential diagnosis from the first beginning with any patient presented with compressing chest symptoms.
We report a case of a 39-year-old man with a symptomatic mediastinal mass.
In the examination of the patient’s medical history in detail in 2013, a chest-X-ray was made due to severe bronchitis symptoms and it had appeared normal (Fig. 1A). In 2017, also a chest radiograph was performed due to the same symptoms but it had shown pulmonary artery enlargement (Fig. 1B). He was admitted to our hospital in 2019 with insidious increase shortness of breath (stage 3 on MMRC), dry cough, chest pain and palpitations.
 Figure1: (A) 2013 (B) 2017 (C) 2019
Figure1: (A) 2013 (B) 2017 (C) 2019
A chest X-ray showed a mass shadow around 7 cm in diameter (Fig. 1C). The contrast-enhanced computed tomography (CT) revealed a heterogeneous mass measuring (7×6×5 cm) in the anterior right mediastinum. It contains bone, fat, soft tissue and calcifications. The right atrium and the superior vena cava are markedly compressed
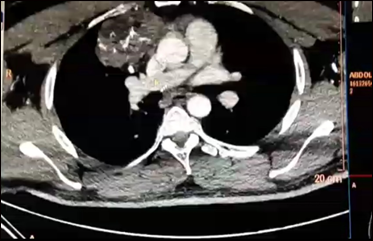
Figure 2: Contrast-enhanced computed tomography shows a heterogenous mass (7×6×5 cm) in the anterior right mediastinum. It is surrounded by a capsule and contains bone, fat, soft tissue and calcifications. The right atrium and the inferior vena cava are markedly compressed.
The lung fields are clear.
With consideration of the tumor size, radiological findings and compression symptoms, a diagnosis of a mature cystic teratoma was highly suspected preoperatively. Because of the tumor’s possibility to be adherent to surrounding structures an open surgery was performed. However, there was no apparent adhesion into major blood vessels or hemorrhage. Subsequently, complete resection of the mass from the anterior mediastinum was successfully achieved. The mass contained high amount of sebaceous and gelatinous materials, as for the inside of the mass hair shafts, teeth and cartilage tissues were identified (Fig. 3).
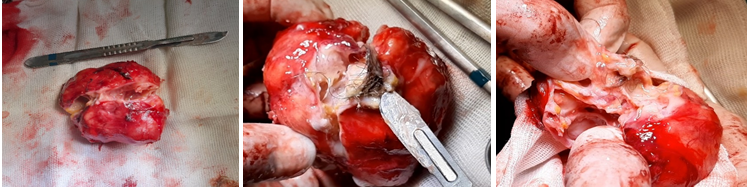
Figure 3: (A) Gross specimen removed from the chest. (B) The tumor contained hair shaft tissues, sebaceous tissue and abundant gelatinous materials. (C) The inside of the mass contained teeth, cartilage tissue and some bone like tissue.
The pathology report confirmed the presence of different mature tissue, including bone marrow, smooth muscle cells and mucinous epithelium (Fig. 4).
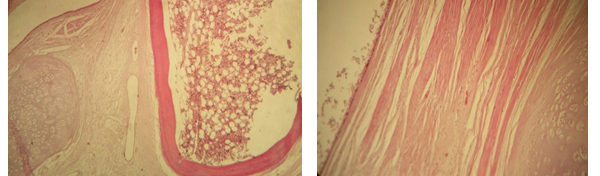
Figure 4: Presence of different mature tissues. (A) Bone marrow, lamellar bone and cartilage. (B) Mucinous epithelium and smooth muscle cells.
The postoperative course was uneventful, without any pulmonary complications. The patient was extubated on day 2 and discharged on the 3rd day after surgery. There was no evidence of recurrence during the 1- and 3-months follow-up evaluations.
Funding: None
We express our sincere appreciation toward Dr. Hossam Mossa; cardiovascular surgeon; for his efforts and support to make this work end.
- Joseph LoCicero III, Richard H.Feins, Yolonda L.Colson, Gaetano Rocco (2018) “Shields’ general thoracic surgery”, 8th edition.
- Chad A Hamilton (2019) cystic teratoma.
- Saba L, Guerriero S, Sulcis R, Virgilio B, Melis G and Mallarini G (2009) ‘‘Mature and immature ovarian teratomas: CT, US and MR imaging characteristics’’ Eur J Radiol 72: 454-463.
- Lewis BD, Hurt RD, Payne WS, Farrow GM, Knapp RH, Muhm JR (1983) ‘‘Benign teratomas of the mediastinum’’ J Thorac Cardiovasc Surg 86(5): 727-731.
- Kim JY. A (2016) ‘‘carcinoid tumor arising from a mature cystic teratoma in a 25-year-old patient: a case study’’ World J Surg Oncol 14:120.
- Varghese TK, Lau CL. The Mediastinum. Townsend CM, Beauchamp RD, Evers BM, Mattox KL, eds (2007) ‘‘Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. 18. Philadelphia’’ PA: Saunders Elsevier, Chap 58.
- Naoki Omachi, Tomoya kawaguchi, Shigeki Shimizu, Tomohisa Okuma, Masanori Kitaichi, Shinji Atagi, Hyunh-Eun Yoon, Akihide Matsumura (2015) ‘‘Life-threatening and Rapidly Growing Teratoma in the Anterior Mediastinum’’. DOI: 10.2169/internalmedicine.54.4622.
- F. Carannantem, L, Frasca, V. Marziali, F. Longo, P. Crucitti (2019) ‘‘Giant mature teratoma in theb thymic tissue removed with uniportal vats approach’’. DOI: 10.1016/j.ijscr.2019.11.031.













