Article / Commentary Article
Lake Erie College of Osteopathic Medicine, LECOM School of Health Services Administration, Adjunct Professor, Health Services Administration & AI in Healthcare.
Dr. Marcos A. Sanchez-Gonzalez, MD, PhD, MSMEd, LSSBB
Adjunct Professor,
Lake Erie College of Osteopathic Medicine
LECOM School of Health Services Administration
Health Services Administration & AI in Healthcare,
4800 Lakewood Ranch Blvd, Suite 2108, Bradenton,
FL 34211.
19 May 2025 ; 11 June 2025
Education remains one of the most underutilized tools in healthcare, despite its proven impact on clinical outcomes. While physicians are expected to teach, few receive training in adult learning principles. Emerging AI beings—adaptive, conversational systems grounded in educational science—offer a scalable medical training and patient engagement solution. These tools extend beyond the classroom, guiding patients through personalized Health Journeys that promote understanding, behavior change, and equity. To truly modernize care, we must integrate AI-driven education into formal curricula and treat patient education as a clinical competency, because informed learners, both doctors and patients, improve the system from within.
Would we allow a schoolteacher to prescribe a medication? Certainly not. Yet in healthcare, we routinely expect physicians to teach patients, students, and residents without formal training in the principles of adult education. This paradox has persisted across generations, even as medical errors and communication breakdowns cost lives (Makary & Daniel, 2016). If education is how we train physicians to practice safely and effectively, how can we treat it as anything less than a clinical tool?
Nelson Mandela once said, “Education is the most powerful weapon you can use to change the world.” In clinical medicine, however, education remains one of the most underutilized interventions. When delivered with the appropriate timing, content, and modality, education should be viewed as a therapeutic instrument no less critical than a prescribed medication. Education influences behavior, enhances comprehension, and fosters long-term engagement, making it a foundational, yet often overlooked, determinant of health outcomes.
Fortunately, we are now witnessing the emergence of a new class of tools that can finally elevate education to its rightful place in clinical care. These tools are not human. They are AI beings—conversational, adaptive, and ethically designed systems that personalize learning for healthcare professionals and patients. Interestingly, medical education has already begun to see the potential of these AI beings (edYOU Los Angeles CA, USA). Our experience with flipped classrooms powered by adaptive platforms shows promising gains in learner engagement, content retention, and real-time feedback. Tools like the Personalized Ingestion Engine (PIE) and Intelligent Curation Engine (ICE) ensure that information is tailored to the learner and delivered safely, free from bias or misinformation (Sanchez-Gonzalez & Terrell, 2023; Chan & Zary, 2019; Lo & Hew, 2023). Across the literature, generative AI has been shown to boost motivation, support active learning, and enable learners to critique and co-create their assessments (Birks et al., 2024; Monzon & Hays, 2025). Strikingly, this is only half the story. The real opportunity lies not just in training better doctors, but in teaching our patients better, too.
Healthcare has long focused on access to care, treatment adherence, and optimizing decision-making through clinical algorithms. However, we have failed to recognize that most healthcare decisions—from managing blood pressure to recognizing signs of depression—are made not in hospitals, but in homes. Furthermore, those decisions are made by patients, often without the guidance they need. What if we treated patient education with the scientific rigor we now demand from our training programs? What if every patient had access to an AI being that could walk them through a diagnosis, a lifestyle plan, or a health goal, with compassion, clarity, and customization?
That vision is no longer speculative. Health Journeys, powered by the same adaptive engines used in education, are beginning to deliver tailored behavioral interventions, digital coaching, and structured learning plans to patients managing chronic pain, mental health conditions, and lifestyle-related diseases. These tools are designed and built not on technological hype, but on the foundations of andragogy—the science of adult learning—while respecting autonomy, adapting to readiness, and offering patients a role not just as care recipients, but as learners in control of their health narrative. Crucially, they are scalable, requiring no additional clinician time, and they promote equity by delivering consistent, accessible guidance regardless of geography, literacy level, or appointment availability.
This moment demands more than admiration for what is possible. It calls for action. If adaptive AI may improve learning, we must advocate for its formal integration into medical training through curricula, accreditation standards, and continuing medical education. Nevertheless, we must go further. Patient education must be treated as a clinical competency, with tools, quality standards, and systems to support it. Competency-based education cannot stop at the bedside; it must extend into the lived environments where patients make daily health decisions.
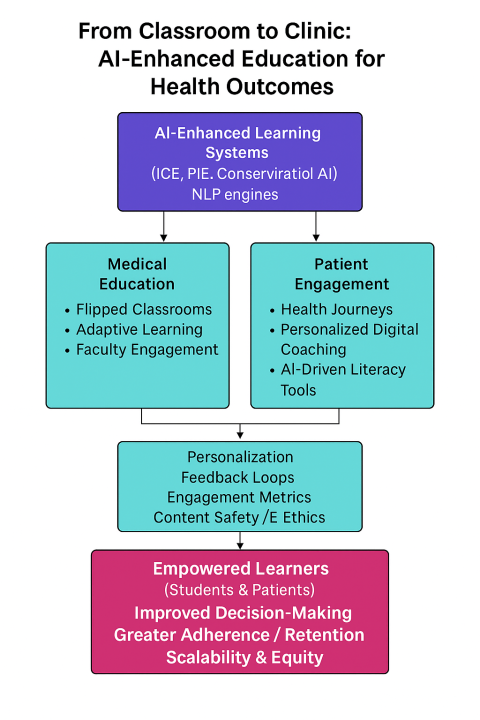 Figure 1: A conceptual map illustrates how AI-driven tools like PIE and ICE enable adaptive learning in medical education and patient engagement, supporting informed decision-making, improved literacy, and scalable health outcomes.
Figure 1: A conceptual map illustrates how AI-driven tools like PIE and ICE enable adaptive learning in medical education and patient engagement, supporting informed decision-making, improved literacy, and scalable health outcomes.
Education is not the responsibility of a department, but rather the foundation of every diagnosis, every conversation, every outcome in medicine. We have built smart hospitals, intelligent EHRs, and algorithmic triage systems. Now we must build the educational layer that makes it all work, because informed doctors and empowered patients do not just use the system better—they change healthcare for the better.
As Mandela reminded us, “Education is the most powerful tool you can use to change the world.” Though he called it a weapon, we choose the word tool because education is not a force of resistance but a source of restoration in healthcare. With AI beings as the instrument, and human health as our greatest treasure, we now have the means to transform care through knowledge, not just for physicians, but for every patient we serve.
- Birks, S., Martin, L., Taverner, T., et al. (2024). Using artificial intelligence to provide a ‘flipped assessment’ approach to medical education learning opportunities. Medical Teacher, 46(1), 1–8.
- Chan, K. S., & Zary, N. (2019). Applications and challenges of implementing artificial intelligence in medical education: Integrative review. JMIR Medical Education, 5(1), e13930.
- Lo, C. K., & Hew, K. F. (2023). A review of integrating AI-based chatbots into flipped learning: New possibilities and challenges. Frontiers in Education, 8, 1–12.
- Makary, M. A., & Daniel, M. (2016). Medical error—the third leading cause of death in the US. BMJ, 353, i2139.
- Monzon, N., & Hays, F. A. (2025). Leveraging generative AI to improve motivation and retrieval in higher education learners. JMIR Medical Education, 11, e54179.
- Sanchez-Gonzalez, M., & Terrell, M. (2023). Flipped classroom with artificial intelligence: Educational effectiveness of combining voice-over presentations and AI. Cureus, 15(11), e48354.













