Article / Case Report
1 St. Joseph’s Medical Center, Stockton, CA.
2Central Valley Eye Medical Group, Stockton, CA.
Dr. Kimberly Cockerham, MD, FACS
Central Valley Eye Medical Group
Plastics-Orbit-Neuro
Medical appointments: 209-952-3700
Cosmetic appointments: 209-952-3705
Cell: 650-804-9270
CVEMG.com
CockerhamMD.com
7 December 2020 ; 15 February 2021
Coronavirus disease 2019 caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has been seen to have varied presentation affecting multiple organ systems. Mucormycosis is a rapidly progressive disease often seen in immunocompromised patients or those with diabetes mellitus with guarded prognosis. This report is based on an interesting case of a 37-year-old man with orbital apex syndrome secondary to mucormycosis and co-infection with COVID-19. We discuss the benefit of administering liposomal amphotericin via retrobulbar injection in addition to systemic antifungals in the setting of rhino-orbital-mucormycosis.
Keywords: Amphotericin, coronavirus, covid-19, orbital apex syndrome, orbital cellulitis, mucormycosis
Methicillin-Resistant Staphylococcus Aureus(MRSA)
erythrocyte sedimentation rate (ESR)
C-reactive protein (CRP)
Relative afferent pupillary defect (RAPD)
cerebrospinal fluid (CSF)
magnetic resonance imaging (MRI)
magnetic resonance venography (MRV)
computerized tomography venography (CTV).
A 37-year-old Hispanic male recently released from prison with a history of positive MRSA status and poorly controlled type 1 diabetes mellitus was admitted for diabetic ketoacidosis. He complained of a two-week history of sinus pressure and headache prior to developing mental status changes. He was found to be COVID-19 positive with elevated ESR (86), CRP (25) and D-dimer (378). On the third day of admission when he was no longer obtunded, he complained of increased left eye pain and swelling.

Figure 1: Complete ptosis with supraduction and abduction deficits of the left eye.
On exam, he had a visual acuity of 20/40 in the right eye, Counting Fingers at six feet in the left eye, without rAPD, 2mm of proptosis, eyelid edema with erythema, and complete ptosis with supraduction and abduction deficits of his left eye (Figure 1).
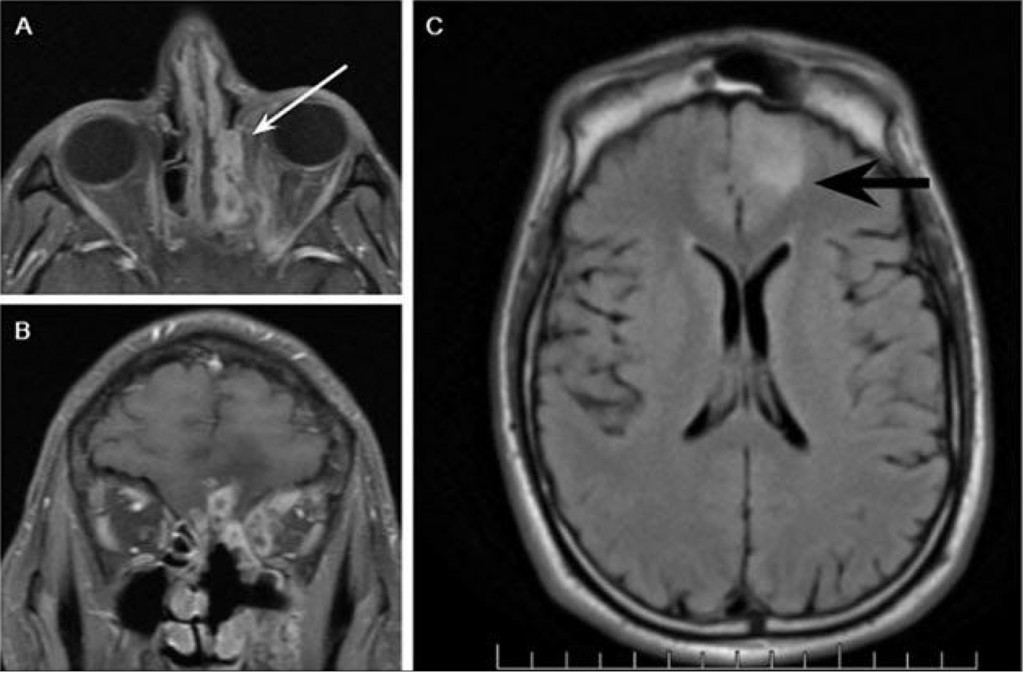
Figure 2 : MRI of the brain and orbits with and without gadolinium for patient post functional endoscopic sinus surgery. A) Axial T1-weighted fat-saturated post-contrast image and B) coronal T1-weighted fat-saturated post-contrast image showing enhancement and inflammatory changes in the left medial rectus with adjacent extraconal enhancing inflammatory densities extending from the left ethmoid sinus (white arrow). C) Axial T2 propeller FLAIR image showing inflammatory enhancement superior to the left cribriform plate with involvement of the inferior aspect of the left frontal lobe and surrounding parenchymal edema (black arrow).
CT of the orbits revealed enhancement of the periorbita along the superior medial margin of the left orbit, mildly displaced medial rectus muscle laterally, and extensive mucosal thickening in the left ethmoid and sphenoid sinuses. (Figure 2) MRI of the orbits revealed a 5mm focally increased T2 signal in the left gyrus rectus. The clinical examination and imaging scans were concerning for a left orbital apex syndrome. The patient was started on Unasyn, Remdesivir and high dose Decadron. Bedside nasal endoscopy revealed an edematous left inferior turbinate with blackened dried blood along the nasal floor. After receiving Decadron, his preseptal cellulitis, ptosis, and motility deficits improved and his visual acuity was 20/40 OS.
The ENT service took the patient to surgery and the middle turbinate was found to be necrotic to the skull base. Preliminary reports showed fungal hyphae consistent with mucormycosis. The patient was started on Amphotericin B and Decadron was discontinued.
However, his ESR, CRP started to trend upward. The patient’s visual acuity deteriorated to 20/400, and his extraocular motility worsened with involvement of CN IV, VI and both the superior and inferior divisions of CNIII with pupil involvement. The patient underwent a MRV and CTV, which were negative for a cavernous sinus thrombosis. A repeat MRI revealed a progressively larger T2 signal abnormality extending from the overlying left gyrus rectus adjacent inferior frontal lobe and new enhancement superior to the left cribriform plate, left medial extraconal fat and medial and superior rectus muscles. He underwent debridement of posterior ethmoids and the sphenoid sinuses with irrigation and amphotericin B. A lumbar puncture was performed and CSF cultures were negative for bacteria or fungus.
Repeat MRI continued to show signs of invasive sinusitis and enhancement extending to the inferior aspect of the left frontal lobe and clivus. He underwent a combined craniotomy and medial orbitotomy under the neurosurgery and oculoplastic service. Intra-operatively, the periorbita, orbital fat and extraocular muscles appeared normal without purulence or necrosis. The gram stain showed rare fungal elements. Liposomal amphotericin was injected into the medial and inferior orbit and via retrobulbar injection. No fungus was identified on the permanent pathology.
Preliminary specimen culture from the sinuses showed Rhizopus species, as well as MRSA, coagulase negative staph, and staphylococcus epidermidis growth. The patient’s postoperative course was complicated by an acute kidney injury secondary to amphotericin B and pre-existing diabetic nephropathy. He was eventually transferred out of the ICU and his vision gradually improved to 20/20 OS six weeks later, but the partial third nerve palsy remained.
Coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has proven to be a complex, challenging illness in its diverse array of presentations and complications, which continue to be under investigation. Ophthalmic manifestations have presented as dry eye, conjunctivitis, ocular pain, and has also been possibly associated with neuro-ophthalmologic and retinal pathologies such as cranial nerve palsies [1], multifocal choroiditis [2] and central retinal vein occlusion [3]. Orbital involvement or associated orbital presentations thus far have not been well documented in literature. One case reported a 60-year-old diabetic patient who was admitted for COVID-19 and received parental meropenem and oral oseltamivir with parenteral methylprednisolone. Over the course of his hospitalization, the patient developed orbital cellulitis, which was biopsy positive for mucormycosis, suggesting that the extensive use of steroids/monoclonal antibodies/broad spectrum antibiotics may lead to or exacerbate pre-existing fungal disease. [4] Presented two unusual orbital presentations of cellulitis in the context of SARS-CoV-2 co-infection, which ended up with negative cultures for any allergic or invasive fungal disease. The combination of systemic immune alterations from the SARS-CoV-2 virus, preexisting co-morbidities and use of immunosuppressive treatments lends itself to an increased risk for secondary infections. As in our case, rhino-orbital-mucormycosis is an emergent, often fatal disease with mortality rates reported up to 80% or more if left untreated and a guarded prognosis even with prompt treatment. Early diagnosis, control of the predisposing diseases, aggressive surgical debridement and administration of systemic and local antifungal therapies are key for improved prognosis.
Several recent studies have suggested that fungal co-infections associated with global COVID-19 may be missed or misdiagnosed [5, 6]. During this pandemic, clinicians should be aware of the increased risk of invasive secondary fungal infections in patients with COVID-19 infection, especially in high-risk patients with pre-existing comorbidities.
None to disclose
- Luís ME, Hipólito-Fernandes D, Mota C, et al (2020). A Review of Neuro-Ophthalmological Manifestations of Human Coronavirus Infection. Eye Brain, 12:129-137.
- Ortiz-Seller A, Martínez Costa L, Hernández-Pons A, Valls Pascual E, Solves Alemany A, Albert-Fort M (2020). Ophthalmic and Neuro-ophthalmic Manifestations of Coronavirus Disease 2019 (COVID-19). Ocul Immunol Inflamm, 28(8):1285-1289.
- Walinjkar JA, Makhija SC, Sharma HR, Morekar SR, Natarajan S (2020). Central retinal vein occlusion with COVID-19 infection as the presumptive etiology. Indian J Ophthalmol, 68(11):2572-2574.
- Turbin RE, Wawrzusin PJ, Sakla NM, et al (2020). Orbital cellulitis, sinusitis and intracranial abnormalities in two adolescents with COVID-19. Orbit, 39(4):305-310.
- Gangneux JP, Bougnoux ME, Dannaoui E, Cornet M, Zahar JR (2020). Invasive fungal diseases during COVID-19: We should be prepared. J Mycol Med, 30(2):100971.
- Song G, Liang G, Liu W (2020). Fungal Co-infections Associated with Global COVID-19 Pandemic: A Clinical and Diagnostic Perspective from China. Mycopathologia, 185(4):599-606.













