Article / Case Report
1NICU Consultant, Maternity Children hospital, Makkah, Saudi Arabia.
2NICU Consultant, Head of department @ Maternity Children hospital, Makkah, Saudi Arabia.
3NICU Consultant @ Maternity Children hospital, Makkah, Saudi Arabia.
4NICU Consultant, hospital, manager of Maternity Children hospital, Makkah, Saudi Arabia.
5NICU Consultant @ king Faisal specialist hospital and research center Jeddah.
6Senior pediatric consultant@ Maternity Children hospital, Makkah, Saudi Arabia.
7Saudi Bord@ Maternity Children hospital, Makkah, Saudi Arabia.
Dr. Najia alhojaili
NICU Consultant
Maternity Children Hospital
Makkah Saudi Arabia.
27 Jun 2021 ; 12 Jul 2021
Our case late preterm 35 weeks. IUGR admitted in NICU as case of late preterm with respiratory distress on noninvasive respiratory support CPAP 5, baby doing well but the problem we cannot wean him from CPAP, he behaves not like 35 weeks, he had a lot of secretion.
Gastroesophageal reflux and esophageal atresia to roll out, baby stayed long time on oxygen take antibiotic and all investigation was done encloud cerebrospinal fluid, urine and blood and serology was sent cystic fibrosis was rollout because the secretion and pneumonia. And vascular ring was rollout, as the baby developed stridor ENT consultant rollout bronchomalacia.
Neonatal pneumonia is lung infection in a neonate. Onset may be within hours of birth and part of a generalized sepsis syn-drome or after 7 days and confined to the lungs. Signs may be limited to respiratory distress or progress to shock and death. Diagnosis is by clinical and laboratory evaluation for sepsis. Treatment is initial.
1. Prolonge rupture of membrane
2. Preterm infant
3. Immune disorder
Baby had pneumonia present with respiratory distress in form of tachypnea, retraction, and desaturation it varies between mild, moderate, and severe, mild respiratory distress respiratory rate more than 60 ppm.
Moderate respiratory distress Respiratory Rate more than 60 ppm with retraction and granting. Severe respiratory distress had Respiratory distress, Respiratory Rate more than 60 ppm. Retracting and desaturation and need respiratory support mechanical ventilator.
Preterm, intergrowth retardation IUGR, 35 weeks delivered to 30 years, G2P1+0, follow up in private hospital, no history of prolonged rupture of membrane, no history of chronic disease baby cried immediately with good Apgar score8,9,9 developed tachypnea Immediately after birth put on CPAP 5with 30% oxygen, blood gas showed mild respiratory acidosis.
Investigation CBC complete blood count was normal. Chemistry was normal.
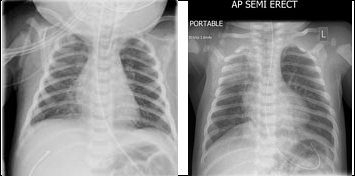
x-ray showed there is haziness in the right upper zone going with pneumonia as baby was not need high oxygen only less than 30% so noninvasive respiratory support was continued, blood culture was taken, and antibiotic ampicillin and gentamycin was started.
2nd day of life we cannot wean him from CPAP. OGT (orogastric tube) stared, and mother was bringing milk.
3rd day of life baby need more oxygen up to 30-35%, and not much clinical improvement so again septic work up was done, blood culture, urine culture, cerebrospinal fluid all culture were no growth and antibiotic Ampicillin. Gentamycin was discontinued and added vancomycin and tazocine.
So, review the history again, take the history from father, he gave history of Covid 19 in early trimester and all the family had Covid 19.
Baby looks well, alert no dysmorphic feature, no rash, Birth weight 2.3 kg looks IUGR baby connected to CPAP 5 Fio2=35%
HR=135ppm, RR=40ppm Temperature =37c Saturation=95-96
Chest decreased breath sound bilateral, no crepitation no wheezing.
Cardiovascular system 1st and 2nd heart sound were normal no murmur, no gallop.
Gastrointestinal system abdomen soft. Liver enlarged 3cm below costal margin, no ascites, and spleen was not palpable. Normal male genitalia. Tone and reflexes were normal.
1. preterm baby with RDS
2. Transient Tachypnea of newborn
3. Sepsis
4. Congenital pneumonia
5. Congenital infection
6. Gastroesophageal reflux
7. Aspiration Pneumonia
8. Cystic Fibrosis
9. Vascular Ring
10. Liver Failure
Complete blood count showed leukocytosis,
Chemistry was normal.
Liver function showed markedly increase enzymes more than ten times, INR was double than normal.
Coagulation profile was prolonged three times.
Blood culture, urine culture, cerebrospinal fluid was no growth.
Serology test sent for hepatitis, Toxoplasmosis, Rubella and Syphilis
x-ray skull done. To roll out any calcification =no calcification
Chest x-ray showed infiltration bilateral.
Baby admitted inside intensive care unit under CPAP 5, with fio2 35%, kept NPO with OGT drain ,1st septic work up was done started on ampicillin and gentamycin.
On 3rd day of life, the infant developed a fever with progressive sign of increased breathing difficulties ,such tachypnea and chest retraction ,but his hemodynamic status remained normal and chest x-ray showed infiltration most probably pneumonic patch ,during visiting time asked father more detail about the history because the mother had follow up in another hospital ,father informed there no history of prolonged rupture of membrane but she had Covid 19 during 1st trimester proved by PCR Test and all his family was positive for COVID 19.So we consult the infectious disease consultant he gave advise no need to take Swab, the mother infected during 1st trimester unlikely shedding of virus stayed for 6month ,so antibiotic ampicillin and gentamicin were discontinued and added tazocine and vancomycin and septic work up were done include blood culture urine culture and cerebrospinal fluid analysis and culture all were no growth, and x-ray chest show pneumonia ,liver enzyme so high we wondering is there relationship between COVID 19 in early pregnancy and pneumonia and liver failure in this infant we did not know especially we did not do PCR test and swab for covid according to infectious consultant ,so we worked in another direction mange the case as liver failure and gave vitamin k intravenous daily 1mg iv od for 3consecutive days, Fresh frozen plasma 15ml/kg over 3hours ,and made consultation to gastroenterology who was gave advise conservative management and daily do coagulation profile and liver function test to do it daily ,infant was not show much improvement especially he develop cyanotic spells during nurse care and a lots of secretion from mouth and from nose and stridor so we asked for cardiology to come and do echocardiogram to roll out vascular ring ,echo cardiogram was done show small PDA ,PFO and gastroenterology came to roll out H- type fistula he advised to call ENT consultant because the infant had stridor although he did not intubation during the course in the hospital ,ENT consultant visualized the focal cord by laryngoscope and a lots of secretion came out removed by suction and send for culture which was no growth.
Baby improved slightly get better, weaned from CPAP, put on nasal canula, received dexamethasone IV injection for 3 doses plus racemic epinephrin inhaler and 3% sodium chloride Inhaler. video fluoroscopy for swallowing test showed sever pharyngeal dysphagia due to the problems 1- aspiration of trace amount liquid 2- weak or ineffective pharyngeal swallow.
1-Frequent oral suction
2-keep good oral hygiene
3-keep the baby on OGT feeding with nonnutritive sucking by using pacifier will enhance the transition from tube to oral feeding. Consult the dietarian to maintain his nutrition, swallowing re -assessment should be after one month for further swallowing management and recommendation.
Mothers with COVID-19 infection may present with obstetrical complications such as preterm labor, premature rupture of membranes, intrauterine growth restriction and neonatal death.
Our case was different, mother got Covid 19 in early trimester and she was complete her pregnancy but the product was late preterm 35 weeks with pneumonia need noninvasive respiratory support and stayed in hospital more than 45 days and liver failure with markedly increase liver enzyme to thousand and prolonged coagulation profile need to receive fresh frozen plasma ,we are wandering if mother got Covid 19,in early trimester, the infection will vertical transmission to fetus and the shedding the infection for long time ,we did not know? Many cohort and case studies have strongly supported the absence of vertical transmission (1) our case had normal platelets but liver enzymes so high suspected liver failure, Finally, the group from Antoine-Béclère Hospital (France) recently reported a proven in utero trans placental transmission of SARS-Cov2 from a pregnant woman infected with COVID-19(2).
We do not know is the virus stayed in placenta for long time and shedding the infection to the fetus because the mother got infection in 1st trimester and after that she recovered completely and continue her pregnancy, we do not put in our mind may be the baby infected that why we did not order for COVID 19 PCR Test and oropharyngeal swab.
In this case if the baby get infection by COVID 19, the mode of transmission is most likely vertical transmission, the absence of visiting of mother to the unit because she was living faraway.
Is the breast feeding is the source of infection we did not know because father brought maternal expressed breast milk and was given to baby through OGT (oral gastric tube, skin to skin contact is not permitted because I mentioned we did not see the mother only father came to visit the baby and he brought the pumped breast milk.
This emphasizes the need for a cautious and close follow -up period for asymptomatic mother who was got COVID 19during pregnancy and delivered normal delivery, is the shedding of virus present and his effect on the newborn or the plumbed breast milk it contains virus we do not know, need more study and more follow up especially in our case baby got pneumonia and liver failure in 1st week and need more respiratory support, in form of high nasal flow should be kept in mind.
The authors declare no conflict of interest.
- Piersigilli F., Carkeek K., Hocq C., van Grambezen B., Hubinont C., Chatzis O., van der Linden D., Danhaive O. COVID-19 in a 26-week preterm neonate. Lancet Child Adolesc. Health. 2020;4: 476–478. doi: 10.1016/S2352- 4642(20)30140-1. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Vivanti A., Vauloup-Fellous C., Prevot S., Zupan V., Suffee C., do Cao J., Benachi A., de Luca D. Transplacental transmission of SARS-CoV-2 infection. Commun. 2020;11: 3572. doi: 10.1038/s41467-020-17436-6. [PMC free article] [PubMed] [CrossRef] [Google Scholar]