Article / Case Report
1MeloNurse at the Federal University of Rio de Janeiro – UFRJ. University Hospital Gafree and Guinle. Specialist by the Multiprofessional Residency Program in Health – UNIRIO. Mastering at PPGSTHE – UNIRIO. Rio de Janeiro – Rio de Janeiro ORCID ID: https://orcid.org/0000-0001-9191-6134
2MacielNurse at Veiga de Almeida University, UVA / RJ Specialist in Nursing In Pediatric and Neonatal Icu – Unyleya, Unyleya Faculty Rio de Janeiro – Rio de Janeiro http://orcid.org/0000- 0003-1092-0911
3Specialist nurse in pediatric, work institution Hospital University Gafree E Guinle
4Nursing Technician to pediatric Hospital University Gafree and Guinle. Titulation: Work Nurse
5Master Nurse, Working institution Hospital Universitário Gafree e Guinle ORCID: https://orcid.org/0000-0001-9191-6134
6Social Assistent of Paliative care of HUGG Specialist in Law and Health – DIHS / ENSP / FIOCRUZ Specialization in Palliative Care – Albert Einstein Institute Master in Bioethics – IMS / UERJ / PPGBIOSRio de Janeiro – Rio de Janeiro
7Physiotherapist, specialist critical care neonatal and pediatric ICU, master in women’s and children’s health, working institution Hospital Universitário Gafree e Guinle in uniti critical care neonatology ORCID: http://orcid.org/0000-0001-9049-9367
8Pediatrician / Neonatologist at the Federal University of the State of Riode Janeiro – UNIRIO. PhD student in Science at PPGENFBIO / UNIRIO. Rio de Janeiro – Rio de Janeiro
9Physiotherapist to critical care Hospital University Gafree and Guinle. Graduation pos in trauma orthopedics by UNAMA and specialist acunpunture
10Coordinating physician of the Prontobaby hospital, physician of the central hospital of the military police
11Routine physiotherapist at Centro Pediatric Hospital da Lagoa, master in women’s and children’s health https://orcid.org/0000- 0002-1180-3795?lang=pt
12Coordinating physiotherapist at the Centro pediatric da Lagoa hospital and Prontobaby hospital, specialist in neonatal and pediatric ICU.
13Physiotherapist, master in women’s and children’s health
14Specialist in gastroenterology, routine at the pediatric ward of Hospital, Gafree and Guinle University
Dr. Cinthia Torres Leite
Physiotherapist
Specialist critical care neonatal and pediatric ICU
Master in women’s and children’s health
Working institution Hospital Universitário Gafree e
Guinle in uniti critical care neonatology
ORCID : http://orcid.org/0000-0001-9049-9367
Brazil
3 December 2020 ; 18 December 2020
To study the case of a patient with Covid 19 with an association for Kawasaki Syndrome whose inflammatory response was moderate and presented in the abdomen mainly in addition to upper limbs and proximal lower limbs.
the information was obtained by reviewing the medical record, photographic record of the diagnostic methods to which the patient was submitted and reviewing the literature.
the reported case and raised publications bring to light the discussion of the treatment of a new, viral situation, Covid 19, which is the disease with systemic inflammation, complicating, in the case studied in Kawasaki syndrome, and showing that, although adopted in a minority of cases, when performed well and in properly treated patients, it is able to obtain satisfactory and long-lasting results with regard to symptom relief and patient improvement.
Covid 19, Kawasaki Disease, Children.
A Kawasaki disease is an acute febrile eruptive disease characterized by systemic vasculitis, particularly in small and medium arteries.
Bearing more than 80% two cases of Kawasaki disease occur in children under 5 years of age, and boys are more prone to Kawasaki disease than boys [Kawasaki et al., 1974; Yanagawa et al., 1995a, b, c, 1995a, 1995b, 1995c, 1996, 1998; Tsuchida et al., 1996].
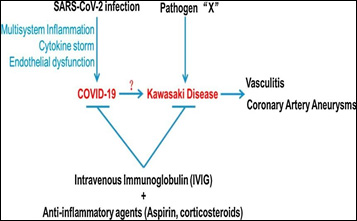
Although or causative agent of the Kawasaki disease is not clear, it is proven that an infectious agent caused or triggered the Kawasaki disease. Besides various pathogens such as some viral agents, these being adenoviruses, pavovirus, Ebstein Bahr among others, recent reports will suggest that heat shock proteins and super antigens produced by bacteria are associated with or development in the Kawasaki teaching [Matsubara e Fukaya, 2007; Nagata et al).
Or human coronavirus (HCoV) is an RNA virus with envelope with a single positive phyta genome [Wege et al., 1982; Lai e Cavanagh,1997]. Several HCoVs have been identified as causative agents of the human common cold, including HCoV- 229E, HCoV-OC43 (OC43), HCoV-HKU1 [Woo et al., 2005] and HCoV-NL63 [van der Hoek et al., 2004]. In 2005, it was reported that a new strain, HCoV – NL63 [Esper et al., 2005b], was possibly associated with a Kawasaki disease, respiratory samples of patients with a Kawasaki disease, in comparison with 1 of 22 (4.5% ) samples of controls from the corresponding country and region [Esper et al., 2005a]. However, many subsequent reports will not be able to confirm the relationship between a Kawasaki ownership and or HCoV-NL63.
O HCoV – 229E was reported for the first time in the 1960s [Hamre and Procknow, 1966] as a common cold inducer HCoV. It’s an Alphacoronavirus, similar to HCoV – NL63. Dijkman et al. [2008] reported that 75% and 65% of infants aged 2.5 to 3.5 years were soropositive for HCoV-NL63 and HCoV-229E, respectively, and that a greater number of infants were soroconverted to HCoVs for 6 years of age. This high prevalence of soropositivity suggests that most of the people present acute HCoV infection during childhood. Therefore, or HCoV is a possible causative agent of Kawasaki teaching, it causes other factors, including genetic background, also may be involved in the development of Kawasaki teaching.
Furthermore, it is proven that the common cold caused by HCoVs generally shows a seasonality of winter, however, Gaunt et al. [2010] report that either HCoV-229E was sporadically detected during the year, but epidemiological surveillance studies for HCoVs were very limited. On the other hand, it has been reported that Kawasaki disease cases increase not see and not winter [Burns et al., 2005]. Therefore, it is necessary to postulate that HCoV-229E is a possible causative agent of the Kawasaki infection of HCoV-229E hair infection during the year.
An epidemic of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), causing COVID-19, is rapidly falling all over the world. Italy was the first European country to be affected, as estimated for the end of February 2020. The city of Bergamo has a higher taxa of infections and deaths in Italy, or that returns to the province of Bergamo a natural epidemiological center where SARS As infections by -CoV-2 appear more often and more evident.
In adults, COVID-19 is typically characterized by severe interstitial pneumonia and hyperactivity of the inflammatory cascade.3, 4 In infants, or respiratory involvement seems to have a more benign course, with almost no death reported in this age group.5, 6, 7 No Therefore, respiratory treatment does not appear to be the only system susceptible to infection by SARS-CoV-2.8 Increasing events suggest that technical damage in COVID-19 is mainly mediated by the immune system of the host.9,10 This teaching is characterized by a storm of cytokines similar to macrophage activation observed in viral-induced hemophagocytic lympho-histiocytes. 11. Despite the fact that it has passed half a century since Tomisaku Kawasaki reported the first time in his 50 cases in Japan, 12 because of Kawasaki’s teaching remains unknown. Hypothesis, more oil does not respond to an aberrant response of the immune system to one or more pathogens not identified in genetically predisposed patients.
Report the case of a patient with Covid 19, whose evolution was for Kawasaki syndrome.
The information contained in this work was obtained by means of a record review, a photographic record of two diagnostic methods, four years or a patient, and was submitted to the literature review.
AFS patient, male, 2 years old, born on 06/05/2018, upon admission to the emergency department of the Centro Pediátrico da Lagoa hospital on 05/25/2020, presenting fever and previous vomiting episodes, also diarrhea and edema to be clarified, Initially, he showed symptoms of impetigo, being treated with benzathine penicillin, he progressed with the injury, therefore, keeping fever. At dawn of the hospitalization, he appears 3 episodes of vomiting and little oil and maternal blood. Evolution for hospitalization in CTI where it remains for 5 days, followed by UI, as an evolution, where it remains for 7 days after completing antibiotic therapy, initially presenting a diagnosis of UTI hospitalization, diarrhea and edema to be clarified, injuries due to prurid scarring and Skin injuries characteristic of Kawasaki syndrome. After conducting sorology for Covid 19 he received a positive diagnosis being defined as Covid 19 and Kawasaki syndrome. He remains a year all 12 days hospitalized receiving hospital discharge on 06/07/2020 in good conditions, together with the genitor.
SatO2 89% -99% FC 128- 110. FR 30-25 Tax 38 – 36.3
AP: MVUA with bilateral wheezing and snoring
PCR = 24 (5/25/2020)
FBC (5/26/2020) = Hto 28.7% Hb 9.8 Hto 28.7%

Hb 9,8 7000 (0/5/0/0/6/39/44/6) PCR 13,3 Plaq 214000
TP 15 TAP 54,3% INR 1,32 PTT 27,0 INR 1,13 PTT 27,0
INR 1,13 PTT rel 0,92
(31/5/2020) hem 4,52/ 12,3/ 37,2% Leuco 11700 Plaq 395000 PCR 1,0
(04/06/2020) hem 4,25/12,2/36,5 Leuco 9500 Plaq 521000 PCR 0,1
(25/5/2020) U 24 C 0,8 Cl 100 Na 133 K 4,4 Ca 8,5 Mg 2,5 P 4,8 Glic 108 Alb
3,5 Tgo 17 Tgp 10 Fa 418 GGT 16 Bt 0,3 Ac Urico 3,4
(04/06/2020) U 28 Cret 0,34 Cl 106 Na 137 K 5 Mg 2,5 P 7,9 Glic 86 Uric acid
2,6 TGO 29 TGP 10 FÃ 377
Total Ptn 7,5 Alb 3,7 Glo 3,8 GGT 10 BT 0,1 BL 0,1 Amylase 47 Lipase 39 URC (25/05) neg
HMC (25/5) neg Stools (26/5) positive Covid neg (29/05)
Children with respiratory failure can manifest the condition of different forms, from mild to moderate and severe manifestations. Most of those infected have an asymptomatic course and numerous false negative cases have been described in molecular tests in this population. Those who develop clinical Covid-19 have fever and cough, few have significant radiological changes, and the prognosis is generally favorable, in contrast to the disease course observed in neonates.
Kawasaki’s disease is an acute febrile systemic infantile vasculitis, which is suspected to be triggered by respiratory viral infections. In the study by O Naim et al.
It was examined whether the ongoing COVID-19 epidemic caused by the severe acute respiratory syndrome (SARS-CoV-2) coronavirus 2 is associated with an increased incidence of Kawasaki disease. From 2005 to 2020, a total of 230 children with Kawasaki syndrome were studied. In the present study, the story of a male patient who presented with initial respiratory failure with rapid progression to skin lesions was described, where red spots were observed in the abdomen, mainly beyond, and upper limb did not progress during hospitalization.
According to Nakamura Y et al, Kawasaki’s disease is an acute febrile systemic vasculitis in childhood that affects the medium and small blood vessels with coronary artery tropism.
The disease is a major cause of heart disease acquired in industrialized countries. For Rolman RC et al 13, there is no specific test to confirm the diagnosis. The diagnosis of Kawasaki disease is based on internationally accepted clinical criteria, 14, 15 combining fever lasting 5 days or more with at least four of the following clinical signs: bilateral conjunctival injection, changes affecting the lips and the oral cavity (inflammation of the mouth and pharyngeal mucosa), polymorphic rash, changes in the peripheral extremities or perineal area and cervical lymphadenopathy of 15 mm or greater. Patients who meet the case definition based on the main clinical findings are considered to have complete Kawasaki disease [1-8].
In our study, we observed a moderate degree of respiratory failure, requiring support in oxygen therapy, maintaining a regular breathing pattern with good chest expansion, but with the use of accessory musculature and slight retraction of the sternal wishbone; equivalent to the picture of moderate respiratory failure as well as the authors Holanda MA (5) te al. describe in their studies. Also according to authors, pediatric respiratory emergencies are among the most frequent causes of hospitalization and deaths in children under 1 year of age. The pediatric population is susceptible to developing severe AKI due to anatomical peculiarities and physiological and immunological characteristics (6) (Brazilian Society of Pediatrics). Thus, in our study, we noticed that the acute respiratory failure generated by contact with the Covid virus 19 evolved moderately with a rapid response to oxygen therapy, as well as secondary conditions such as Kawasaki syndrome evolved mildly with complete improvement of the condition.
It is worth mentioning that this study is extremely relevant due to the current situation where a good outcome was verified without the need for invasive treatment or more severe supports for the clinical manifestation described here.
- Wu Z, McGoogan JM et al (2020) Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020; 3231239
- Parri N, Lenge M , Buonsenso D et al (2020) Children with Covid-19 in pediatric emergency departments in Italy. N Engl J Med. 2020; (published online May 1.). DOI:10.1056/NEJMc2007617 Crossref
- Nakamura Y , Yashiro M , Uehara R , Oki I , Watanabe M , Yanagawa H (2008) Epidemiologic features of Kawasaki disease in Japan: results from the nationwide survey in 2005–2006. J Epidemiol 18: 167-172.
- Holman RC , Curns AT , Belay ED, Steiner CA , Schonberger LB (2003) Kawasaki syndrome hospitalizations in the United States, 1997 and 2000. Pediatrics 112: 495-501.
- NETHERLAND MA, et al. (2001) Noninvasive positive pressure ventilation in patients with acute respiratory failure: factors associated with failure or success. J. Pulmonology 27(6): 301-309.
- BRAZILIAN SOCIETY OF PEDIATRICS. Accute breathing insufficiency. Scientific Department of Intensive Care; 2017. n.2.
- FONSECA JG, et al (2013) Assessment and initial management of acute respiratory failure in children. Rev Med Minas Gerais 23 (2): 2.
- HAMMER J (2013) Acute respiratory failure in children. Ped Resp Rev 14: 64-69.













