Article / Research Article
Silesian Eye Treatment Center, Poland
Adam Cywinski
Head of the Center
Silesian Eye Treatment Center
44-240 Zory
Poland
20 November 2020 ; 10 December 2020
The article analyses 22 cases of severe impairment of vision to far distances for no apparent reason. Visual impairment was observed regardless of patients’ age and type of eye defect diagnosed, with the majority of people suffering from myopia and accompanying astigmatism. The exclusion of causes related to the cornea and retina, optic nerve damage and the lack of visible pathologies of the lens in the physical examination did not allow for the determination of the cause of deterioration in visual acuity to far distances despite good vision to near distances. The results of examinations using iTrace indicated the lens as the cause of visual impairment despite the apparent lack of opacity and other pathologies within it. The results of examinations in the field of Higher Order Aberration, Opacity Map, Modulation Transfer Function™ and their graphical presentation using the Dysfunctional Lens Index™ module were analysed. Low values of visual contrast sensitivity and high values of higher order aberrations for the internal optics were observed, with the correct values for the cornea. The more pathological the results of the visual contrast sensitivity and higher order aberration, the lower the values of visual acuity to far distances. In most cases removing the dysfunctional lens and replacing it with an artificial lens allowed for a significant improvement in vision to far distances while maintaining proper vision to near distances. The procedure was performed on patients over 18 years of age. The medical history in the study group may indicate a congenital nature of the abnormal structure of the lens. Thus, it is necessary to consider verification of the diagnosis made in some patients, pointing to a new disease entity, i.e. congenital lens dysfunction.
Keywords: Lens Dysfunction, Itrace, Decreased Vision, Amblyopia
The term dysfunctional lens syndrome refers to changes that occur in the crystalline lens after the age of 40. The main purpose of introducing this term was to better understand the relationship between changes in visual quality caused by the aging (clouding) lens. Fernandez et al. mention, among others, the appearance of higher order aberration (HOA) and light scattering as the consequences of the aging process, and draw attention to the diversified influence of the opaque lens on the quality of vision [1,2]. Rezza Sedaghat et al. described a case of an unclear reduction in the quality of vision in a patient without visible cataract or other ocular causes. In the summary of the article, the authors noted the presence of high order aberrations (HOA) from internal optics, including the crystalline lens, which were not compensated by the cornea, and pointed to this as the cause of poor visual acuity [3]. Similar cases of poor visual acuity caused by the presence of a transparent but dysfunctional crystalline lens were presented by Steve Dewey in his presentation The ‘Dysfunctional’ Dysfunctional Lens Patient [4].
The aging process of the lens is not the only cause of deterioration of vision. Other causes include the abnormal structure of the lens, including spherophakia, the posterior lenticonus and its subluxation (ectopia lentis) [5-7]. What do these pathologies have in common? First of all, they are easy to diagnose using the simplest examination method, i.e. direct biomicroscopy. Another common feature is that visual acuity can be improved after surgical removal of the defective lens. Prost points to enormous benefits of the procedure to remove the lens with the posterior lenticonus performed in children [5]. Treatment of lens ectopy in the case of severe subluxation requires its surgical removal, as does the presence of cataract. It is difficult to list all the ophthalmic causes of decreased visual acuity. Thanks to modern technology, most of them can already be diagnosed, and all changes which can occur with time can be followed up. Taking into account lens pathologies direct biomicroscopy allows for the detection of mainly those lesions that are visible. In some cases, the lack of visible pathologies in the lens structure is not synonymous with their absence. In such cases, diagnostics should be extended. Devices using ray tracing technologies, including those that assess the presence of higher order aberrations (HOA), allow for the detection of lens pathologies. Not every device that examines the presence of HOA allows for such analysis. The condition is that the corneal aberrations have to be separated from those in the internal optics. One of such devices is iTrace. This device combines, among others, the function of corneal topography and aberrometer. Thanks to its structure, iTrace allows for the assessment of many important details of the optical system of the eye. In addition to the function of separating the corneal aberrations from those in the internal optics, the device can also assess corneal topography, measure eye defect, the axis of vision, kappa and alpha angles as well as the eye’s accommodation ability. When assessing the condition of the lens, the Opacity Map and Modulation Transfer Function™ (MTF) modules as well as HOA analysis allow for the condition to be analysed in terms of its structure and impact on the quality of vision. This data is extremely useful in preoperative qualification for cataract removal, refractive lens replacement, or the differentiation of poor quality of vision observed after artificial lens implantation. In iTrace corneal wave front is based on Zernike calculation of the refractive map using the Snell’s law of refraction. Generally, in this device (…) the aberrations of the Internal Optics are obtained by subtracting of the Corneal Wavefront Aberrations of corneal aberration from the Total Ocular Aberrations”, said Karolline Maya Rocha, MD, in her presentation “A diagnostic solution to drive premium cataract surgery” [8-11]. Additionally, using the Dysfunctional Lens Index™ (DLI) module we obtain a graphic simulation of the obtained results (letter “E”), which shows how the cornea and the internal optics commonly and separately affect the quality of the received image. The above functions can be extremely useful in diagnosing unclear cases of visual impairment. In some patients in whom corneal pathologies, visible lens pathologies (cataract, spherophakia, lenticonus or lens dislocation), pathologies of the vitreous, retina and optic nerve were excluded making a correct diagnosis becomes a challenge. It is not uncommon that the diagnosis is incorrect in the presence of visual impairments associated with decreased visual acuity. Amblyopia, macular dysfunction, dysfunction of the optic nerve or keratoconus are the most common diagnoses, the accuracy of which can be undermined and considered erroneous upon deeper analysis of the results obtained. Taking into account the definition of amblyopia, this diagnosis should not be made when visual acuity to near distances is normal, and only the quality of vision and visual acuity to far distances are significantly reduced [12]. In such conditions, in the absence of visible causes of poor vision, special attention should be paid to the condition of the lens and its possible adverse influence on the visual function.
Between April 2019 and May 2020, 12 people (22 eyes) were examined using iTrace due to an unclear cause of poor visual acuity to far distances that could not be corrected in any way.
The main impulse to create the above group was the case of a 40-year-old man. This patient came for consultation because of poor visual acuity to far distances, which had been observed practically since childhood. Despite the lack of features of keratoconus, confirmed many times using corneal topography examination in another clinic, the patient was treated based on the diagnosis of keratoconus for 5 years. Numerous physical examinations, including an assessment of the condition of the lens, vitreous body, cornea and retina, did not reveal any pathologies that could cause poor vision to far distances. The results of the examinations involving intraocular pressure, visual fields, ERG VEP, and MRI were normal. The patient denied having any systemic diseases.
The patient was diagnosed with severe myopia and corneal astigmatism. The obtained values of best correction visual acuity (BCVA) to far distances are as follows: right eye: 0.7 with correction -12Dsph -2.7Dcyl, left eye: 0.8 with correction -15Dsph -4.0Dcyl, examined using Log MAR charts. Visual acuity to near distances, without correction, as assessed using Snellen charts was normal in both eyes. The axial length (right eye: 24.2 mm, left eye: 24.35 mm) indicated refractive type myopia. In order to assess the influence of the lens on the quality of vision, an iTrace examination was performed. Corneal topography as part of the iTrace examination once again ruled out the presence of keratoconus. The obtained MTF, DLI™, HOA results clearly indicated the lens as the cause of deterioration in the quality of vision, despite the absence of any visible pathologies in its structure. The patient underwent surgery to remove the dysfunctional lens followed by the implantation of premium class lenses: Mplus toric, i.e. bifocal toric lenses with an addition of +3.0Dsph, manufactured by Oculentis. Seven days after surgery, the patient stated that he did not remember ever having such good vision to far distances. Visual acuity of both eyes without correction improved by 4 rows, reaching the value of 0.3 on Log MAR charts. Visual acuity to near distances remained consistently normal.
Taking into account the above case, only the patients who met the following criteria were analysed:
- A significant disproportion between visual acuity too far and near distances.
- Poor visual acuity to far distances, despite the best correction of the diagnosed eye defect.
- Normal visual acuity to near distances, examined without or with the best correction, depending on the diagnosed eye defect.
- No visible pathologies were found during the examination of the cornea, lens, vitreous body, retina and optic nerve. Examinations were conducted before and after pupil dilation.
The absence of pathologies within the eye structures were confirmed by the following examinations: direct and indirect biomicroscopy of the anterior and posterior segment of the eye, corneal topography (iTrace), static visual field – neurological type, OCT of the disc and the macula, intraocular pressure.
Each patient who met the above criteria was examined using iTrace. The examination was repeated three times one by one. The presence of high HOA values in the corneal examination also excluded patients from the study group.
The following values were analysed: Dysfunctional Lens Index™ (DLI), Opacity Map, Modulation Transfer Function (MTF) and higher order aberrations (HOA), including mainly Coma and Trefoil aberrations. HOAs were assessed at a constant pupil diameter, i.e. 3mm, although the average pupil size values were much higher. The results obtained from the examination of the cornea and internal optics were analysed separately and as a common result (TOTAL EYE).
When it was confirmed that the lens is the probable cause of poor visual acuity to far distances, patients were qualified for the removal of the dysfunctional lens followed by premium quality lens implantation. Patients under 18 years of age were not qualified for lens removal surgery at that time.
The results of examinations of 15 people (22 eyes), including 4 women, were analysed. Of this group, 7 patients (5 bilaterally) underwent surgery to remove the dysfunctional lens. The average age of the patients was 38 years, ranging from 9 to 44 years. Refractometry performed before the procedure showed values of eye defect ranging from -22Dsp -1.75Dcyl to + 7.0Dsph -1.75Dcyl, the highest astigmatism of the optical system reaching the value of +7.75Dcyl. As previously mentioned, all patients had normal visual acuity to near distances, obtained with or without correction (depending on the diagnosed eye defect), and low visual acuity to far distances. The majority of the group consisted of patients with high and moderate myopia, with comorbid astigmatism. The youngest participant, a 9-year-old boy, had mixed myopia tending towards refractive myopia and astigmatism in both eyes, with the following values: right eye (RE) -7.5Dsph -3.75Dcyl, left eye (LE) -9.5Dsph -3.5Dcyl, with the axial length of 25.34 of the right eye and 24.72 of the left eye. Hyperopia, always with comorbid astigmatism, was diagnosed in 4 people, unilaterally.
Sex, age, eye defect, axial length, DLI™ value and the diagnosis made due to poor vision quality are presented in Table 1.
| Sex/age (years) | Eye defect (dioptres) Sph/Cyl |
BCVA to far (Log MAR) | BCVA to near (Snellen) |
biometry | DLI™ |
|---|---|---|---|---|---|
| M/41 | +5.0/+2.75 anisometropy | 0.5 | 0.5 | 21.59 | 6.25 |
| m/40 | +6.5/+1.5 anisometropy | 0.6 | 0.75 | 21.45 | 4.28 |
| m/9 | -7.5/-3.75 | 0.7 | 0.5 | 25.34 | 0.92 |
| -9.5/-3.5 | 0.6 | 0.5 | 24.92 | 2.25 | |
| m/41 | -14 | 0.8 | 0.5 | 26.8 | 2.3 |
| -14/-1.25 | 0.8 | 0.5 | 27.07 | 1.61 | |
| m/31 | -16/-3 | 0.5 | 0.5 | 29.6 | 1.63 |
| -18/-3 | 0.5 | 0.5 | 29.8 | 0.85 | |
| m/23 | -21/-2 | 0.9 | 0.5 | 29.71 | 0.65 |
| -21/-2 | 1.0 | 0.5 | 29.93 | 0.35 | |
| m/40 | -12/-2.75 | 0.7 | 0.5 | 24.2 | 0.43 |
| -15.5/-4 | 0.7 | 0.5 | 24.35 | 0.42 | |
| k/30 | -16.5/-5.75 | 1.0 | 0.75 | 27.35 | 1.8 |
| -10.75/-4.25 | 0.6 | 0.5 | 24.04 | 1.05 | |
| k/61 | -19/-3 anisometropy | 0.8f | 0.5 | 33.2 | 0.49 |
| m/22 | -22.0/-1.75anisometropy | 0.7 | 0.5 | 30.2 | 0.93 |
| k/38 | +7.25/+1.75 anisometropy |
0.4 | 0.5 | 20.7 | 3.82 |
| m/50 | +5.0/+7.75 | 0.6 | 0.75 | 23.16 | 7.18 |
| m/44 | +3.5 anisometropy |
0.7 | 0.5 | 24.2 | 2.43 |
| m/14 | -12/-4 | 0.6 | 0.5 | 28.2 | 1.71 |
| -15/-4,5 | 0.5 | 0.5 | 29.1 | 1,22 | |
| m/26 | -19/-3,5 anisometropy | 0.7 | 0.5 | 30.21 | 0.55 |
Results of iTrace examinations were analysed. The analysis involved the results of all patients, regardless of whether or not the dysfunctional lens was removed. The above examinations were not repeated after the procedure due to the different types of implanted intraocular lenses. The lenses differed in structure (monofocal lenses, monofocal toric lenses, bifocal lenses, bifocal toric lenses and those using EDOF technology).
HOA, Coma and Trefoil, averaged values obtained from the internal optics, the cornea and the total value are presented in Diagram 1.
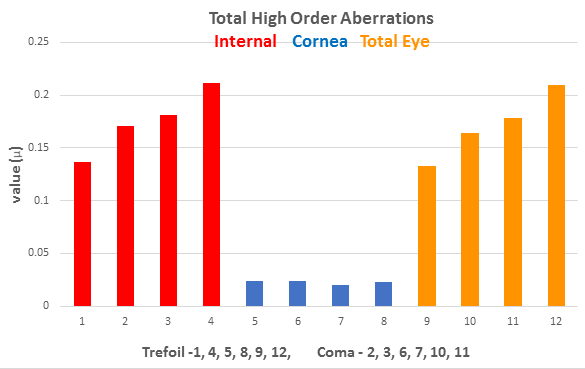
Average values of higher order aberrations, i.e. Coma and Trefoil for the internal optics (lens), the cornea and their total value.
The graph shows that significantly increased HOA values were obtained for the internal optics (lens) and as the total value of aberrations of the entire eye, i.e. obtained from the cornea and the internal optics. The higher the aberration values, the greater the problems with the quality of vision. The highest Total Internal HOA values in the scope of Trefoil reached 0.700µ, and in the case of Coma even up to 0.910µ. Similar HOA values were obtained by summing the aberrations of the internal optics and the cornea (Total Eye). In the case of the cornea, the values for Trefoil did not exceed 0.059µ and for Coma 0.079µ, so they were minimal, close to zero. Interpreting the obtained result, it can be clearly stated that high HOA values came from the internal optics (lens). Another conclusion is the lack of correction of the Total Internal HOA by the structure of the cornea, which occurs in some cases [13].
Modulation Transfer Function (MTF). The three main factors that influence the quality and determine the ability to distinguish very fine details include the optical system of the eye, the condition of the retina and the visual pathway with the visual cortex. The quality of the optical system of the eye, including mainly visual contrast sensitivity is best defined by the Modulation Transfer Function. The quotient of the contrast sensitivity of the obtained image to the contrast sensitivity of the observed item is defined by the MTF. Therefore, the obtained results of this function inform us about the image quality that can be generated by individual elements of the optical system, i.e. the cornea (MTF Cornea) and the internal optics, mainly the lens (MTF Internal), and their common result (MTF Total Eye).
The average MTF values for the cornea, the internal optics and the total value are presented in Diagram 2.
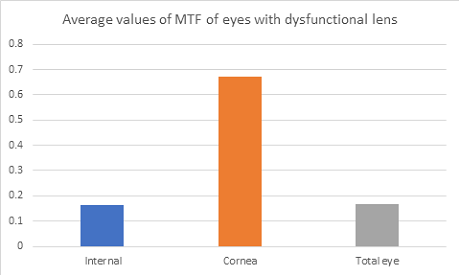
Low MTF values correlate with poor quality and contrast sensitivity. High MTF values allow us to expect good quality of vision. In the discussed group, low MTF values for the internal optics were observed, which adversely affect the MTF of the entire optical system of the eye (MTF-Total Eye) despite obtaining high MTF values from the cornea. The MTF values presented in the form of a graph had a distinctive shape, i.e. a practically flat line for MTF Internal and MTF Total Eye and high values obtained for MTF Cornea (Graph 1).
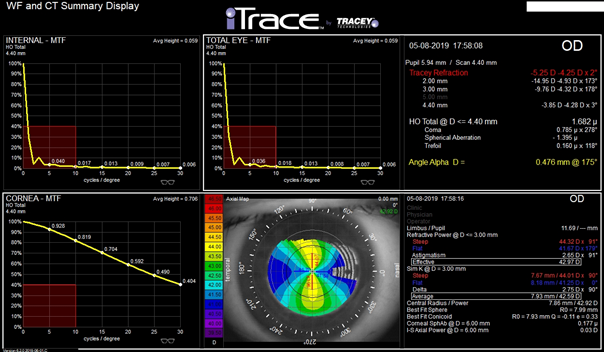
Graph 1. MTF values presented in the form of a graph. Typical result for lens dysfunction syndrome, i.e. low, incorrect Internal -MTF Internal and Total Eye-MTF values and high, correct MTF Cornea-MTF values.
Interpretation of the result – the quality of vision is significantly reduced as a consequence of the presence of pathologies within the lens.
Dysfunctional Lens Index™ (DLI). An index introduced by the inventors of iTrace. Its value is the resultant of internal aberrations, MTF or loss of contrast sensitivity. Pupil size also influences (compensates) the contrast sensitivity values [9].
Correlations between axial length, MTF™ and DLI™ in the study group were analysed.
A correlation was found between the axial length and DLI™ (Diagram 3). Low DLI™ values correlated with high values of the axial length, while in the case of a short axial length the DLI values were high.
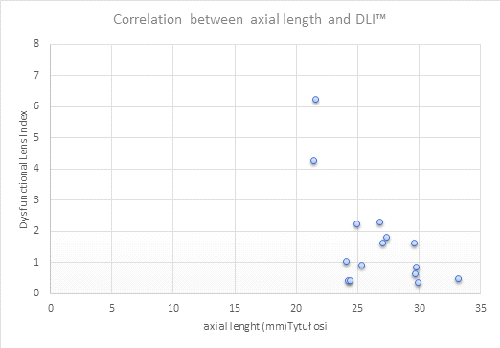
Diagram 3: Correlation between DLI and axial length (mm)
Opacity Map. A value that shows numerically and graphically how much laser energy sent from 128 independent points of iTrace reaches the retina. In the presence of cataract, taking into account the varying degrees of lens opacity, the graphical result of this examination reflects the differences in lens opacity using colours.
In the study group, despite the lack of lens opacity, the average value was 2.1, in the range from 0.5 to 4.0; however, the value ‘0’ indicates the absence and ‘5’ the presence of total opacity [14]. The obtained values could erroneously indicate the presence of lens opacities, which, however, were not present in any of the patients. It can be assumed that the complex structure of a completely transparent, although dysfunctional lens may also cause the appearance of higher values.
In the assessment of, among others, the influence of the lens structure on the quality of the results obtained using iTrace is based on two panels: Dysfunctional Lens Analysis for the MD (medical doctor) and Dysfunctional Lens Analysis for the Patient. The first one includes, among others, average values of MTF and DLI™ (Graph 2).
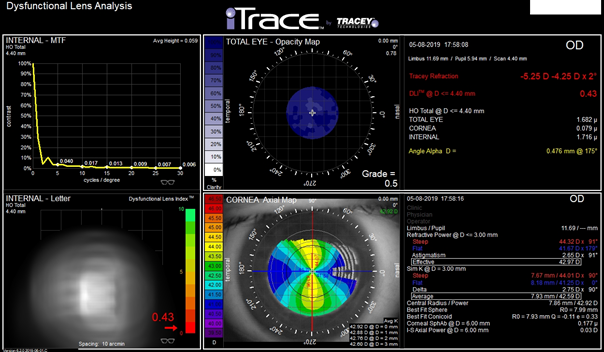
Graph 2: Dysfunctional Lens Analysis for the MD. Among others, graphic representation of MTF Internal, image of the letter “E” adequate to the obtained results in the scope of HOA and Opacity Map in one place
A panel Dysfunctional Lens Analysis for the Patient shows in graphical form -“E” letter a values of HOA achieving from examination of the Cornea and Internal separately and their’s common results – Total Eye. This common result reflects quality of vision of this patient. [9] (Graph 3)
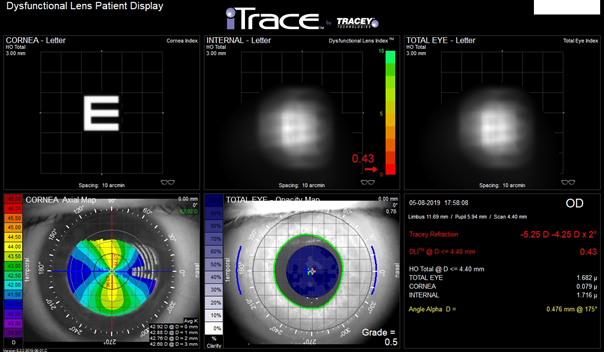
Graph 3: Dysfunctional Lens analysis for the Patient. Image of the letter “E” in the quality reflecting higher order aberration (HOA) values. In this example the abnormal result comes from the Internal and is not corrected by the result achieved from the Cornea, therefore the common result (Total Eye) is also abnormal and reflects the response from the Internal.
Visual acuity to far distances was measured using Log MAR charts, and visual acuity to near distances – using Snellen charts. All patients, except for one, underwent surgery at the private Silesian Eye Disease Treatment Centre in Zory. Surgeries were performed by Adam Cywinski, MD. The surgery to remove the dysfunctional lens was performed in 7 patients, including 5, in whom the surgery was performed bilaterally.
When selecting the lens for implantation, several parameters were taken into account, i.e. the type of eye defect and pupil size. The alpha and kappa angles, the position of the visual axis were obtained using iTrace. The role of the economic factor in lens selection was minor. In the case of myopia, efforts were made to select lenses that allow vision to near distances to be retained and vision to far distances to be gained without the need to use additional correction. Astigmatism above 0.75 dioptres was corrected using toric lenses.
Therefore, the following were implanted: 4 Mplus toric lenses (bifocal with addition to near distances +3.0Dsph), 2 Soleko Evolve lenses (EDOF with addition +2.75Dsph), 1 Mplus Comfort lens (bifocal with EDOF and addition +1.5Dsph), 2 Soleko toric (monofocal), 1 Mplus lens (bifocal with addition +3.0Dsph).
The examinations were performed before and 3 months after the surgery. Visual acuity improved in all cases. The patient with high myopia and astigmatism (RE -13.0Dsph -1.75Dcyl, LE -14.0Dsph -1.25Dcyl), who decided to undergo surgery in a different centre, as part of his insurance, had a monofocal lens implanted bilaterally. Even though visual acuity to far distances improved by 20 letters in both eyes, the patient was not entirely satisfied with the effect. His dissatisfaction resulted from the loss of vision to near distances without correction, which was caused by the calculation of the artificial lens up to the value causing emmetropia.
The comparison of the average value of the best corrected visual acuity (BCVA) before and 3 months after the procedure, without correction (BVA) is shown in Diagram 4.
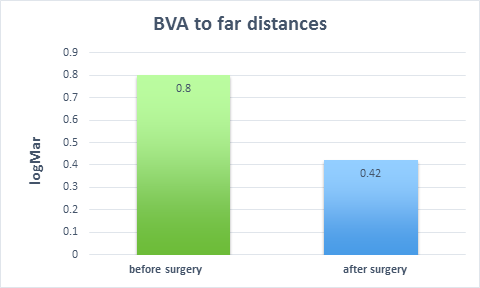
Diagram 4: Average values of BCVA, achieved before and BVA 3 months after the removal of the dysfunctional lens.
The average improvement in vision to far distances reached almost 4 rows, which is about 20 letters. The greatest improvement in vision to far distances was 6 rows, i.e. 30 letters. The smallest improvement was 1 row, i.e. 5 letters. In the case of the latter, the HOA values from the internal optics were only slightly worse (lower) than the Corneal HOA.
None of the patients achieved a 100% improvement in vision to far distances.
In two patients who underwent the procedure, there were additional reasons which influenced achieving improvement of postoperative visual acuity. In the case of a 23-year-old patient with bilateral high myopia at the level of -22.O D/-2.0Dcyl, it was nystagmus and the presence of idiopathic active CNV, requiring implementation of anti-VEGF therapy. Despite the above, removal of the dysfunctional lens improved visual acuity to far distances from 0.9 for RE and 1.0 for LE to 0.5 for RE and 0.6 for LE postoperatively. Visual acuity to near distances was unchanged in both eyes – D-0.5. Another patient, a 30-year-old woman was diagnosed with a dysfunctional lens and a preoperative eye defect of -16.5Dsph/-5.75Dcyl in RE and -10.75/-4.25 in LE. The lesser improvement of postoperative visual acuity to far distances in the left eye resulted from retinal detachment, requiring posterior vitrectomy. Nevertheless, vision to far distances improved from 1.0 to 0.3 in RE and from 0.6 to 0.4 in LE. Postoperative visual acuity to near distances was D-0.5 in RE, and D-0.75 in LE.
Visual acuity to near distances achieved after the procedure remained unchanged in all patients (eyes) and was normal.
Subjective vision improvement was achieved in each case. Patients reacted with euphoria to regaining vision to far distances. The words “I don’t remember seeing so well” were often repeated.
The analysis of the obtained results allows us to draw one important conclusion. An “abnormal” crystalline lens can influence the quality and level of visual acuity, despite the fact that direct biomicroscopy does not reveal any pathologies in its structure. This is a very important observation which allows us to understand and explain why a patient with normal visual acuity to near distances has poor visual acuity to far distances, when no pathologies are revealed in the examination of particular elements of the eye.
The lack of correct diagnosis results in the use of the most likely one. In the case of lens dysfunction, patients who had normal vision to near distances and poor quality of vision to far distances were most frequently diagnosed with amblyopia. Retinal dysfunction, optic nerve abnormalities or cerebral defect were diagnosed in people with high or moderate myopia. An extreme case was the diagnosis of keratoconus in the patient with normal cornea confirmed several times by corneal topography.
Taking into account the achieved results presented in this article, more detailed examination of the lens should be introduced mainly for the two following reasons:
- When there is a large disproportion in visual acuity; vision to near distances is normal, while vision to far distances is abnormal, poor.
- When the available examinations assessing the function of particular eye structures, which can influence vision, do not show any pathology.
In the case of a large disproportion in vision to far and near distances, the diagnosis of amblyopia and its treatment in a way typical for amblyopia is not the right course of action. First, the dysfunctional lens should be removed, and then treatment improving vision to far distances should be implemented.
If we want to prove that the lens, which appears “healthy” in direct biomicroscopy, is dysfunctional, we have to use devices, which allow for examinations of higher order aberrations to be conducted and for contrast sensitivity to be measured. The ability to separate the corneal response from the response from the internal structures of the eye constitutes a necessary function of such a device.
Diagnosis of a dysfunctional lens should not be treated using methods recommended for amblyopia. A dysfunctional lens requires surgical treatment. Most of the patients in the study group had high myopia additionally accompanied by astigmatism. The presence of such eye defect cannot explain the poor quality of vision to far distances maintaining normal vision to near distances. In some patients a dysfunctional lens was diagnosed in the eye with hyperopic astigmatism and was observed unilaterally. One might suppose that unilateral hyperopia at the level of +7.25Dsph +1.75Dcyl will result in severe amblyopia, even more so if the eye has not undergone correction. In the case of the patient with the above defect, best correction visual acuity to near distances was normal (D-0.5, Snellen). Visual acuity to far distances reached 0.4. The DLI value reached up to 3.82, and HOA were abnormally high.
Referring to the failure to achieve normal visual acuity to far distances after the removal of the dysfunctional lens, this condition can be explained by the inability to “teach” the brain the correct interpretation of the image received. In most patients, the lens dysfunction was removed around the age of 40. However, due to the existence of a lens dysfunction, in such a case amblyopia could not be diagnosed [12].
An additional undeniable benefit of removing the dysfunctional lens is removal of eye defect, often very severe and significant anisometropy.
Analysing the results of iTrace examinations, the MTF function – assessment for higher order aberrations including DLI™ – is most appropriate and valuable for the detection of invisible, hidden lens pathologies.
The presence of a significant disproportion between normal visual acuity to near distances and reduced, sometimes to a great extent, visual acuity to far distances, in the absence of tangible reasons for such a condition, including pathological changes of the crystalline lens, should be a factor initiating diagnostics for lens dysfunction.
Such diagnostics should be carried out in all disputable cases regarding the cause of the visual impairment, also in children. Early diagnosis of a dysfunctional lens allows us to avoid inconvenient and ineffective eye treatment recommended for amblyopia. The diagnosis of congenital lens dysfunction as the cause of poor vision quality will allow for the only appropriate treatment to be implemented, i.e. its surgical removal at the appropriate time. Taking into account the available devices that allow for the “detection” of lens dysfunction, iTrace examinations, including functions that assess the presence and scope of higher order aberrations, including MTS™ and DLI™, allow for the detection of lens dysfunction despite the absence of any pathologies in direct biomicroscopy of the eye.
- Fernández J, Rodríguez-Vallejo M, Martínez J, Tauste A, Piñero D (2018) From Presbyopia to Cataracts: A Critical Review on Dysfunctional Lens Syndrome. J Ophthalmol. 2018; 2018: 4318405. Published 2018 Jun 27.
- Dysfunctional Lens Syndrome, a New Way to Educate Patients. AAO 2018 Daily, Oct 14, 2016,
- Mohammad Reza Sedaghat. Hamed Momeni- Moghaddam. Shehzad S Naroo. Hossein Ghavamsaeedi. Alireza Vahedi (2018) Dysfunctional lens syndrome, Int Ophthalmol. 2018 Aug; 38(4):1759-1763.
- Steve Dewey (2015) The “Dysfunctional” Dysfunctional Lens Patient. ASCRS 2015 iTrace Users Meeting. Part 2 of 2 with
- Marek E (2018) Prosthetic posterior cone of the lens – the results of surgical treatment in children Posterior lenticonus – the results of surgical treatment in children. OphthaTherapy 2018; 1(17): 39-45. DOI: 10.24292/01. OT.310318.06
- https://eyewiki.aao.org/Ectopia_Lentis
- S Khokhar. G Pillay. S Sen. E Agarwal (2018) Clinical spectrum and surgical outcomes in spherophakia: a prospective interventional study. Eye (Lond) 32(3): 527– 536.
- Qiao L. Wan X. Cai X. et al. (2014) Comparison of ocular modulation transfer function determined by a ray-tracing aberrometer and a double-pass system in early cataract patients. Chin Med J (Engl) 127(19): 454-3458.
- Karolinne Maia Rocha (2017) Tools that can guide decision-making. Make the most of diagnostic devices to choose the best options for patients with presbyopia. Ophthalmology Management 21 page(s): 22. 24. 26. 27.
- Ayushi Sinha, Siddhi Goel, Vinay Gupta, Devesh Kumawat, Pranita Sahay (2019) iTrace – A Ray Tracing Aberrometer, Delhi Journal of Ophthalmology 30(1) July- September 2019.
- Karolinne Maia Rocha (2015) A Diagnostic Solution to Drive Premium Cataract Surgery. Presentation during ASCRS 2015 iTrace Users Meeting. Part 1 of 2 with.
- Rebecca S (2015) Braverman Introduction to Amblyopia. Academy of Ophthalmology. Clinical Education. OCT 21. 2015.
- Suliman A, Rubin A (2019) A review of higher order aberrations of the human eye. African Vision and Eye Health 78(1).
- http://www.traceytechnologies.com/Tutorial_DLI_ web.pdf













